Introduction: A story that starts with pain
Once upon a time, a 67-year-old patient came to our clinic, Facialia, in Silla, Valencia, seeking relief from unbearable pain in tooth 1.4. What she found was more than an immediate solution: a complete transformation of her oral health. This isn’t just a case; it’s proof that with science, technology, and a dedicated team, any dental problem can have a happy ending.
Wisdom teeth: invisible enemies?

Wisdom teeth might seem harmless until they start wreaking havoc. In this case, the teeth had deep cavities, were poorly positioned, and caused irritation to the mucosa. Additionally, the patient had localized periodontitis and a white lesion on her left cheek. These challenges required more than a simple treatment—they needed an evidence-based and personalized approach.
The diagnosis: knowing the enemy
Our team conducted a comprehensive examination, identifying:
- A root fracture in tooth 1.4.
- Cavities and mobility in the wisdom teeth (1.8 and 2.8).
- A white lesion on the left cheek.
- Early localized periodontitis in molars.
With these findings, we developed a strategic and personalized plan to address each issue effectively.
The treatment: science in action
At Facialia, every step of our treatment is grounded in research and evidence. Here’s what we did:
- Oral hygiene education: We taught advanced brushing and flossing techniques.
- Scaling and root planing: To combat inflammation and subgingival biofilm.
- Wisdom teeth extraction: Using modern protocols to minimize pain and accelerate recovery.
- Biopsy of the white lesion: We confirmed it was benign and continued removing irritants.
Why Facialia is your best choice in Silla, Valencia
At our dental clinic, we offer:
- Cutting-edge technology: From digital X-rays to advanced surgical tools.
- An expert team: Combining technical expertise with compassionate care.
- Customized plans: Every treatment is tailored to your specific needs.
The outcome: a renewed patient
After completing treatment, our patient not only said goodbye to pain but also regained confidence in her smile. The inflammation subsided, the lesions were controlled, and her oral health was strengthened. What began as an emergency ended as a complete transformation.
Your story can change too
At Facialia, we know that removing wisdom teeth can mark the beginning of a new chapter in your oral health. If you’re ready to take that step, we’re here to help. Book your appointment at facialia.com and start your own transformation story.
A Journey to a Healthier Smile: The Story of a Brave Patient
Once upon a time, a patient walked into our clinic with a sharp pain in her upper jaw. She pointed to tooth 1.4, where the discomfort seemed to come from. Little did she know, this visit would mark the beginning of her journey toward a healthier and happier smile.
The First Clues: Digging Deeper
As we started to examine her case, we uncovered a series of challenges that explained her discomfort. Let’s take a closer look at what we found:
In the Upper Jaw
- First, we discovered a vertical root fracture in tooth 1.4—the main culprit behind her pain.
- Then, we noticed her wisdom teeth were causing trouble. They had cavities, were positioned awkwardly, and even rubbed against her cheek, creating irritation.
- Finally, her restorations needed improvement. They were no longer doing their job effectively.
In the Lower Jaw
- Tooth 4.4 showed a periapical lesion—an infection at the root. This tooth was also weakened by a condition called condensing osteitis.
- Her wisdom tooth at 4.8 was impacted and causing additional strain.
- To top it off, she had localized bone loss due to chronic periodontitis, a gum disease that had slowly been taking its toll.
These discoveries painted a clear picture of why the patient was in pain. But her story didn’t stop there—her background added another layer of complexity.
A Peek Into Her Past
The patient, a 67-year-old retiree, had been married for 30 years. While she had no major allergies, her medical history revealed that she was managing hypercholesterolemia with medication. She also came from a family with a history of rheumatoid arthritis, colon cancer, and heart disease.
One bright spot was her decision to quit smoking 10 years ago. However, she still enjoyed a daily glass of wine, which can sometimes affect oral health.
When it came to dental care, she admitted that her hygiene routine wasn’t the best, and her last dental visit had been over a year ago.
The Examination: Piecing It All Together
During the orofacial exam, we noted several important details:
- Her jaw opening was slightly limited, but her chewing muscles were strong.
- Her tongue was prominent but healthy.
- Her saliva production was good, and her oral tissues looked healthy—except for one concern.
A white lesion on her left cheek caught our attention. It was located where her upper and lower molars touched.
Diagnosing the Problem: Connecting the Dots
After piecing together all the clues, we identified several key issues:
- Gum Recessions: Her gums were receding by 1–2 mm in some areas.
- Tooth Mobility: Some of her teeth, like 2.8 and 1.8, were loose.
- Periodontitis: She had an early stage of gum disease localized in her molars.
- Tooth Decay: Decay and mobility were also affecting her wisdom teeth.
- White Lesion: This well-defined patch required further investigation.
- Vertical Fracture: Tooth 1.4 had a fracture running deep into the root.
The Mystery of the White Lesion
The white lesion on her cheek was a bit of a puzzle. We considered several possibilities:
- Lichen Planus: This condition usually appears as white striations, but it’s typically bilateral—not unilateral like her lesion.
- Candidiasis: While this fungal infection can create white plaques, it wasn’t a match because her lesion couldn’t be scraped off.
- Leukoedema: This condition often affects people of African descent and disappears when the cheek is stretched. But our patient didn’t fit this profile.
In the end, the lesion was most likely leukoplakia, a condition that can sometimes indicate irritation or other underlying issues.
Planning the Next Steps: A Personalized Treatment Plan
Every journey needs a plan, and this one was no exception. Here’s how we mapped out her treatment:
Phase One: Building Healthy Habits
We started by focusing on behavior changes and better oral hygiene. The goal was to empower her to take control of her oral health.
- Education: We taught her proper brushing and flossing techniques and recommended using plaque-detecting tablets to ensure thorough cleaning.
- Lifestyle Changes: We encouraged her to moderate alcohol consumption and reinforced the importance of staying smoke-free.
- Professional Cleaning: We performed a deep clean using airflow technology to remove plaque and tartar.
Phase Two: Addressing the Lesion
If the white lesion didn’t improve within three months, we planned to remove it using a scalpel. Other options like laser therapy or cryotherapy were also on the table.
Phase Three: Resolving Dental Issues
- Tooth 1.4: This fractured tooth would be extracted, with plans for a dental implant after a three-month healing period.
- Tooth 4.4: We treated the condensing osteitis with a root canal and monitored its progress.
- Restorations: Poorly fitting seals would be replaced to improve function and aesthetics.

•

O.P.G. of first check-up
Periapical X-rays:
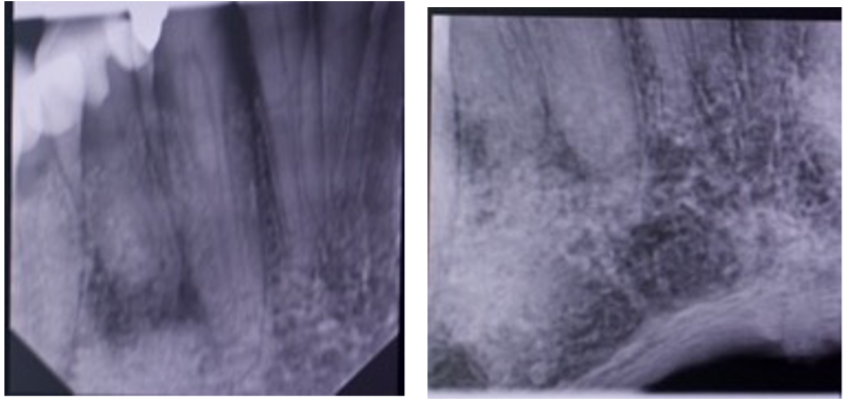
Periapical of tooth 4.4
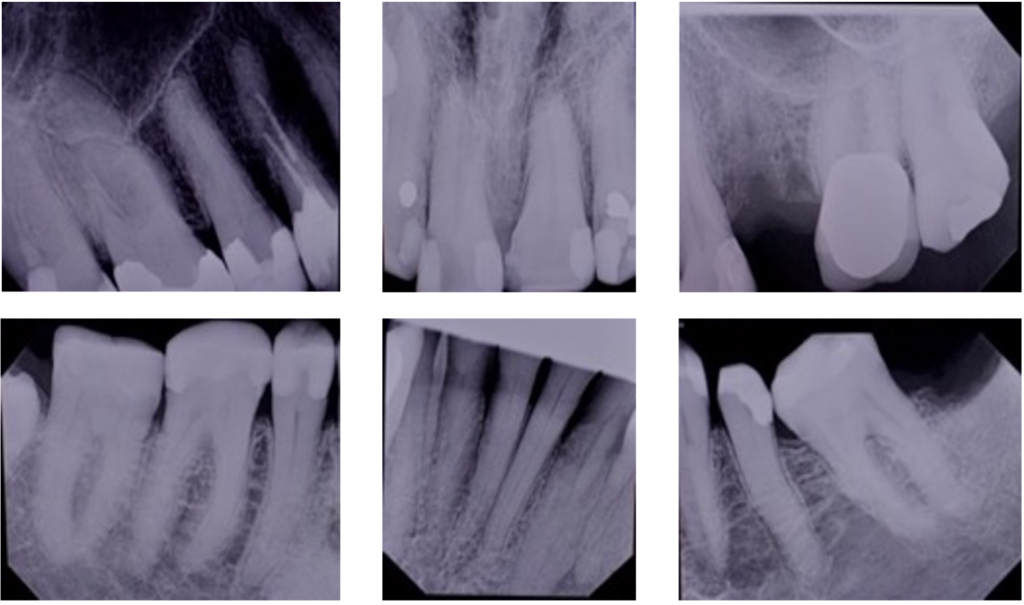
Periapical series
The Initial Diagnosis: Setting the Stage
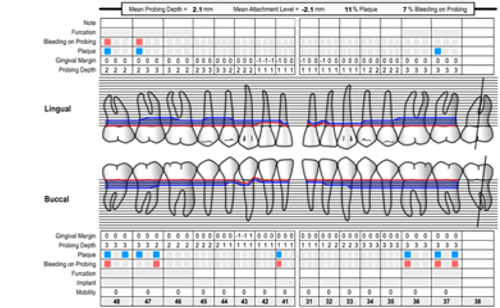
When the patient first arrived, her periodontal chart revealed some trouble areas:
- Attachment Loss (C.A.L.): Most molars showed 3 mm loss, while the front teeth had 2 mm.
- Bleeding and Plaque: Found throughout the mouth, signaling the need for better oral hygiene.
- Gum Recessions:
- Lingual recessions of 1–2 mm (Miller Type I) on the front lower teeth.
- Buccal recessions of 2 mm on teeth 1.3, 2.3, and 4.3.
- Tooth Mobility: Teeth 2.8 and 1.8 were shaky, with a mobility degree of 2–3.
- Periodontitis: Initial signs localized in the molars, classified as Stadium II and Grade A.
Clearly, this was no small challenge, but every challenge is an opportunity to make a change!
First Steps: Education and Motivation
Before any treatment, the patient needed the right tools and knowledge. She was taught how to brush and floss effectively, with an electric toothbrush recommended for its superior plaque removal power.
To make oral hygiene easier and even a bit fun, plaque-detecting tablets were suggested. These colorful tools showed her where she could improve after brushing.
The patient also learned about the negative effects of smoking and drinking. With resources like Slutta.no and studies by experts such as Pinto-Filho et al. (2018), she discovered how quitting these habits could transform her oral and overall health.
Scaling and Root Planing: The Deep Clean
Next, it was time for some serious cleaning! Scaling and root planing tackled the bacteria and buildup deep below the gumline. To ensure thorough disinfection, the treatment included:
- Irrigation with 0.12% chlorhexidine and hydrogen peroxide.
- A powerful antibiotic duo: Amoxicillin 250 mg and Metronidazole 500 mg, taken three times daily for five days.
The goal? Reduce bleeding, control plaque, and shrink those deep gum pockets to less than 4 mm.
The Wisdom Teeth Saga
Sometimes, teeth become troublemakers—and that was the case with the patient’s wisdom teeth. The upper and lower third molars (1.8, 2.8, and 2.4) were causing trauma and gum irritation.
The solution was clear: remove the troublemakers. The extractions went smoothly, followed by antibiotics to promote healing and prevent infection.
A Special Case: Tooth 4.4
Tooth 4.4 presented a unique challenge with condensing osteitis and an apical lesion. After careful evaluation, endodontic treatment (root canal therapy) was performed to save the tooth. Following a proven method from Eliasson et al. (1984), the team decided to monitor its healing progress.
Restoring the Smile: Future Plans
As part of the long-term plan, tooth 1.4 (which had a maladaptive filling) was scheduled for extraction. After allowing two months for healing, a dental implant will be placed to restore both function and aesthetics.
Phase Two: Mastering Periodontal Care
With Phase One complete, the focus shifted to controlling bacteria and preventing future issues. This step included advanced treatments like:
- Adjunctive physical or chemical agents.
- Local or systemic antimicrobials to keep bacteria at bay.
The results? The patient’s gums were healthier, bleeding was under control, and pockets were reduced to less than 4 mm.
Supportive Periodontal Care: Long-Term Success
Now that her gums were stabilized, the patient entered the maintenance phase. Regular check-ups and cleanings ensured her oral health stayed on track.
If any signs of disease appeared during these visits, the team was ready to take swift action with re-treatment or additional care. The key to success was maintaining good habits and regular dental care.
A Brighter Future: Dental Implants and Renewed Confidence
Once the bone in the area of tooth 2.4 had healed, a Biomed BOPT 4/3 10 mm implant was placed. This marked a turning point in the patient’s journey—a step toward a fully restored and confident smile.
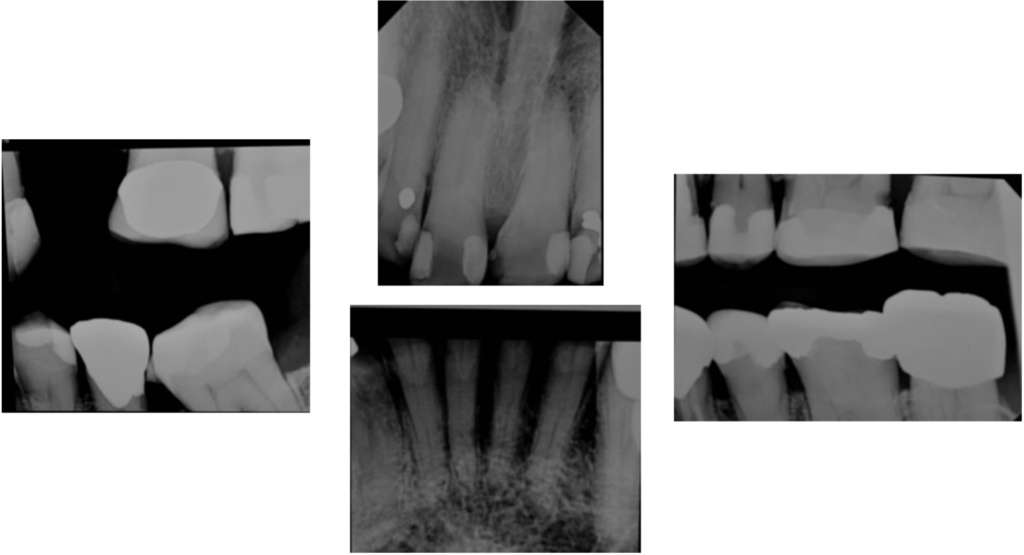
Photos after teeth extractions

2. Options for Treatment of the white lesion
In this case, treating the white lesion eliminated the factors that irritate the mucosa. If, after two months, this lesion grows or presents symptoms, an excisional biopsy will be performed.
- The convenience: Conservative Treatment: Treatment will be done if it does not work.
- The inconvenience: We are not doing an excisional biopsy. We could be skipping an essential step since leukoplakia is a premalignant lesion. However, when it is well-defined, it has a low malignancy index.
Regarding condensing osteitis, the treatment was endodontic treatment.
- The convenience of this option is that it is not an aggressive treatment, which only affects tooth 4.4.
- The downside could be that it did not work and that the tooth had to be extracted.
Photo of the white lesion and broken tooth 2.4

Photos of the white lesion

Surgery and Treatment Details: A Comprehensive Path to Recovery
Step 1: Initial Observations and Action Plan
The journey started with a clear focus on addressing the persistent white lesion and improving the patient’s overall oral health. To polish the restorations on the posterior teeth, the patient was referred back after three weeks. Unfortunately, the lesion showed no improvement during this time.
To rule out complications like yeast infections that might mimic or aggravate conditions such as lichen planus, Clotrimazole (10 mg troches) was prescribed. The patient took five tablets daily for 14 days, as supported by research from Holmstrup and Dabelsteen (2016) and Hellstein and Marek (2019).
Step 2: The Wisdom Teeth Dilemma
After the Clotrimazole treatment, the lesion remained unchanged, but further investigation revealed that trauma from erupted wisdom teeth was worsening the situation. The decision was made to extract the problematic wisdom teeth (2.4, 2.8, and 1.8).
Following the extraction, amoxicillin 500 mg was prescribed—one tablet every eight hours for seven days—to prevent infection. The patient was then scheduled for a follow-up.
Addressing Tooth 4.4: The Next Step
Tooth 4.4 required endodontic treatment to ensure its longevity. The patient was motivated to continue her oral hygiene routine, laying the foundation for successful outcomes.
Lifestyle Counseling: A Holistic Approach
Recognizing the broader impact of lifestyle choices on oral health, the patient was educated on the harmful effects of tobacco and alcohol. Resources such as Slutta.no were recommended to aid in smoking cessation.
The patient was also informed of studies like Pinto-Filho et al. (2018), which highlight the correlation between alcohol dependence and tooth loss. With this knowledge, she was empowered to make healthier choices, further supporting her dental and overall health.
Re-evaluation: A Turning Point
After scaling and root planing, the patient’s oral health showed marked improvement:
- No periodontal pockets greater than 4 mm with bleeding on probing.
- No deep pockets ≥6 mm.
- No pain in the previously treated area of tooth 1.4.
With the primary therapy goals achieved, the patient moved to the next phase of treatment.
Prognosis: Moving Forward with Caution
The prognosis for the patient remained uncertain due to:
- Persistent plaque buildup risks.
- Challenges posed by the white lesions on the left and right cheeks.
However, her commitment to oral hygiene and the retention of interproximal bone provided a silver lining. With plaque levels reduced to below 30% and periodontal pockets under 4 mm, she was ready to enter Phase 4 of her treatment plan.
Phase 4: Supportive Periodontal Care
The focus of this phase was maintaining stability through regular preventive and therapeutic interventions tailored to the patient’s periodontal health. Key aspects of supportive periodontal care included:
- Continuous monitoring for recurrence of disease.
- Regular oral hygiene education.
- Biopsies and diagnostics when lesions persisted or worsened.
Despite earlier trauma from posterior cusp restorations, a biopsy of the white lesion was conducted, confirming the need for further care.
Implant Placement: A New Foundation
Once the bone at the site of tooth 2.4 had healed, a Biomed BOPT 4/3 10 mm implant was placed. This marked another step in restoring the patient’s functionality and aesthetics.
Join Us on Your Journey to Better Oral Health
This patient’s story is a reminder that oral health is about more than teeth—it’s about embracing change, addressing challenges head-on, and committing to better habits.
If you’re facing similar dental concerns or simply want to improve your smile, we’re here to help. Visit us at Facialia.com or come to our clinic in Silla, Valencia, where we specialize in advanced dental treatments and personalized care.
Start your journey today—because every smile deserves a happy ending!

The biopsy was sent to Oslo Universitetssykehus:
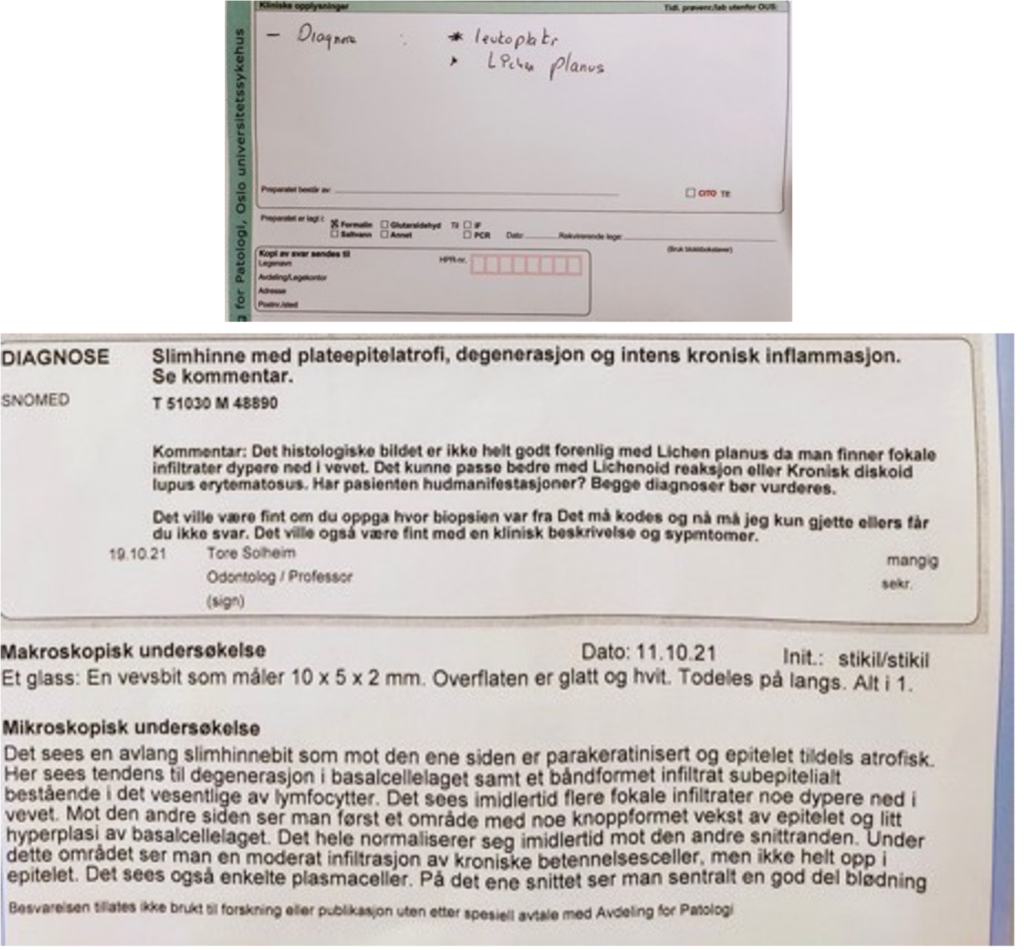
What is chronic discoid lupus erythematosus?
“Discoid lupus erythematosus (DLE) is a chronic skin condition of sores with inflammation and scarring favouring the face, ears, and scalp and, at times, on other body areas. These lesions develop as a red, inflamed patch with a scaling and crusty appearance”. This is written in the American Osteopathic College of Dermatology (AOCD).
Periodontal re-evaluation
To perform the periodontal evaluation, the following treatments were performed:
- Period chart; control plaque; cleaning with scaler and airflow.
UP:
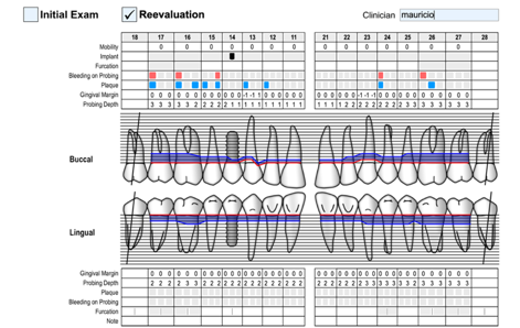
DOWN:
Intraoral photography.

Orthopantomography.
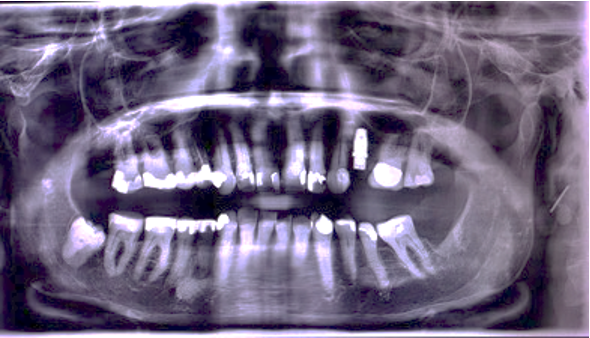
Intraoral photo.
A Patient’s Journey: From Challenges to Smiles
Setting the Goals: The Beginning of a New Chapter
Every journey starts with a plan, and this patient’s story was no different. From the very first visit, we set clear, achievable goals to guide her toward better oral health:
- Control bleeding and plaque to reduce plaque levels to 25%.
- Achieve pocket depths under 4mm to ensure her gums are healthy and strong.
- Eliminate discomfort and bad breath so she could smile confidently without hesitation.
With these goals in mind, the patient embarked on her oral health journey. She started brushing her teeth three times a day for one minute each time and flossing daily. Her commitment began to pay off, as both her bleeding and plaque levels decreased significantly. This was a promising start to her transformation!
A Key Milestone: Placing the Implant at Tooth 1.4
At tooth 1.4, the stage was set. With enough bone already present, it was time to act. A precise punch was made, and a Biomed 3i BIOPT 4/3 x 10 implant was placed seamlessly. To support the healing process, a healing abutment was installed, which also served as a scan body for future steps.
This marked a key milestone in her treatment, but the journey was far from over. The patient will return in six months for a follow-up and periodontal maintenance if needed.
Unexpected Challenges: The Uncertain Prognosis
Life, like a story, often throws unexpected twists. In this case, the patient’s journey took a turn with the discovery of chronic discoid lupus erythematosus. Although the diagnosis added complexity to her case, the patient remained resilient.
Remarkably, she felt fine—no pain, no discomfort, and no troubling symptoms. She continued following her oral health routine diligently, showing that even in the face of uncertainty, perseverance can lead to progress.
The Mystery of the White Lesion
The plot thickened when a white lesion appeared on her cheek. Initial steps to address it—like removing predisposing factors such as cheek-biting trauma—didn’t yield the results we hoped for. A biopsy was performed to rule out anything serious. Thankfully, there were no signs of malignancy, bringing a sigh of relief.
Still, we referred her to an endocrinologist for further investigation. The results confirmed her lupus diagnosis, prompting immediate treatment to manage the disease and prevent further complications.
Managing Lupus: A Lifelong Commitment
As Okon and Werth (2013) explain, chronic discoid lupus erythematosus cannot be cured, but it can be managed effectively. The patient began a treatment plan that combined sun protection education with topical and systemic therapies. With this approach, she could control symptoms and continue her journey toward better health.
Tooth by Tooth: Her Dental Prognosis
Every tooth has its own story in this patient’s journey:
- Tooth 4.4: In need of root canal treatment, this tooth’s future depends on the success of the procedure. Its prognosis could go either way, but we remain optimistic.
- Tooth 2.7: A leaky reconstruction needs to be replaced. If root canal treatment is unnecessary, this tooth has a good chance of recovery. However, calcified root canals could complicate the outlook.
- The Rest of Her Teeth: Thanks to her improved brushing technique and commitment to plaque control, the remaining teeth have a healthy prognosis, considering her age and periodontal status.
The Happy Ending: A Smile Worth Fighting For
This story is a testament to resilience and teamwork. With guidance, proper care, and determination, the patient has overcome significant challenges on her path to a healthier, more confident smile. Her journey isn’t over yet, but every step brings her closer to the happy ending she deserves.
Begin Your Journey Today
If you’re facing similar challenges or simply want to improve your oral health, we’re here to help. Visit us at Facialia or our clinic in Silla, Valencia, where we specialize in personalized dental and periodontal care. Let’s start your story together and create a smile that lasts a lifetime!
Explore more at facialia.com and take the first step toward your new smile!
Re-evaluation
What Happens During Maintenance Check-Ups?
During the first eight months of 2022, our patient attended quarterly appointments. Each visit included the following:
- Targeted cleaning: Scaling and root planing for areas prone to plaque buildup, such as the lower incisors and molars.
- Plaque control education: Personalized advice on improving oral hygiene habits.
- General cleaning: Using advanced tools like air polishers for a thorough clean.
These visits allowed us to monitor her progress and address potential issues early, ensuring her oral health remained stable.
Challenges Along the Way
In November 2022, the patient experienced a setback when her 2.4 implant failed. The root cause was identified as low T lymphocyte levels, a factor in her overall health. Rather than rushing into further treatment, we chose a cautious approach, scheduling reimplantation for April 2023 after her immune system stabilized.
Reassessing and Moving Forward
At her most recent check-up, we focused on keeping her oral health on track:
- Conducted plaque control evaluations to refine her hygiene routine.
- Polished existing dental restorations and targeted cleaning with airflow tools.
- Noted improvements, such as the complete disappearance of a previous mucosal lesion on her left cheek, with the right lesion remaining stable and symptom-free.
Why Maintenance Matters After Wisdom Teeth Removal
Wisdom teeth removal is just the first step toward a healthier smile. Long-term success depends on consistent follow-ups, expert monitoring, and personalized care plans. At Facialia, we combine modern technology and experienced professionals to ensure you maintain optimal oral health.
Start Your Maintenance Journey with Us
Whether you’ve recently undergone wisdom teeth removal or need ongoing care, Facialia in Silla, Valencia, is here to help. Book your appointment at facialia.com and take the next step in protecting your smile.
Wisdom Teeth Removal and Beyond
At Facialia, wisdom teeth removal is only the beginning. With a focus on maintenance and prevention, we ensure your smile stays healthy for years to come. Visit us in Silla, Valencia, and experience expert care tailored to your needs.
Mucosa photo right side

General prognosis
Her hygiene has worsened, with widespread plaque. Bleeding in less than 30% of the teeth.
She continues to attend his maintenance consultations and is waiting to have the implant again from 2.4 if his doctor allows us; otherwise, other alternatives will be studied, such as making a ceramic bridge from 23 to 25.
Her general prognosis is uncertain since her health has recently decreased in the last year.
Teeth prognosis
They have a good prognosis; she has no pain, no caries, and the recessions have no symptoms.


