Regenerative periodontal surgery and bone regeneration are essential tools in modern periodontal treatment. They are especially useful when we have a self-contained defect, that is, a deep bone pocket surrounded by bone walls. In this clinical case at Facialia, our clinic in Silla (Valencia), we used regenerative periodontal surgery and bone regeneration to save key teeth in a complex periodontitis patient.
Because of the patient’s behaviour, fears and risk factors, the treatment was not simple. However, with a clear plan and step-by-step periodontal treatment, it was possible to improve his gum health and stabilise several teeth.
Patient background and main periodontal complaint
Social and medical profile
To begin with, the patient was a 46-year-old man who worked as a CEO. He drank wine daily, around eight glasses per week. In addition, his family history included diabetes, alcoholism and depression.
From a dental point of view, he had known periodontitis since he was a teenager. As a result, he had been attending periodontal maintenance for more than ten years. He usually came to the dentist every five months.
Main reason for consultation
In the last five months, he had noticed something new. When he pressed on the gum above the upper left canine, pus came out. This sign worried him, although he still did not like the idea of surgery.
Previously, several dentists had already told him that he needed resective surgery on many posterior teeth, because pockets were deeper than 5 mm. Nevertheless, he always chose only “maintenance visits” and refused surgical treatment.
Behavioural challenges and initial periodontal assessment
Treatment tolerance and anxiety
One of the biggest challenges in this periodontal treatment was his behaviour. He was extremely squeamish and anxious. Every time we needed to give local anaesthesia, he asked to stop and meditate for a moment. Therefore, each maintenance or scaling visit required around two hours.
On top of that, he suffered from claustrophobia. Because of this fear, he found it very hard to stay in a small X-ray room with the door closed. Consequently, taking radiographs was a slow and delicate process.
Clinical and periodontal findings
Despite these limitations, we managed to perform a clinical exam and several periapical X-rays. The periodontal chart showed:
- General probing depths of 4–5 mm.
- Deeper pockets in molars and in the area between 2.3 and 2.4.
- Clinical attachment loss greater than 5 mm in several teeth.
- Generalised bleeding and visible plaque.
- Thin periodontal biotype and localised recessions.
Altogether, these signs indicated generalised periodontitis stage 3, grade C, which means advanced periodontal disease with a higher risk of progression.
Phase 1: non-surgical periodontal treatment and motivation
Improving hygiene and risk factor control
First, we started Phase 1 periodontal treatment, which focuses on behaviour change and supragingival plaque control. In this step, we:
- Taught him proper brushing and flossing techniques.
- Recommended an electric toothbrush, since it can reduce plaque more effectively than a manual one.
- Suggested plaque-disclosing tablets so he could see where he was missing areas.
In addition, we talked about alcohol and tobacco. We explained, in simple words, that these factors increase the risk of tooth loss and worsen bone loss. As a result, the patient started to understand that periodontal treatment was not just “a cleaning”, but a way to avoid losing teeth.
Response after Phase 1
After several weeks, we re-evaluated his gums. Some areas improved slightly, but deep pockets and suppuration were still present, especially between the upper left canine and premolar (2.3–2.4). Because of this, we decided to continue to Phase 2 and clean below the gum line.
Phase 2: scaling, root planing and periodontal re-evaluation
Subgingival instrumentation
Phase 2 periodontal treatment focuses on subgingival instrumentation. In other words, we clean the roots under the gum. During this phase, our goals were clear:
- Reduce plaque and bleeding to less than 25%.
- Lower pocket depths to under 4 mm where possible.
- Avoid deep pockets of 6 mm or more with bleeding.
- Reduce bad smell and pain.
To achieve these aims, we performed scaling and root planing under local anaesthesia. As usual with this patient, we needed extra time, calm explanations and pauses to manage his anxiety.
Unfavourable results and new symptoms
After this, we scheduled a periodontal re-evaluation. Unfortunately, the results were not good enough. Several deep pockets remained, and a fistula appeared between 2.3 and 2.4, releasing pus when pressed.
At first, the patient still resisted the idea of surgery. However, his partner commented that his breath and taste were unpleasant, and she did not want to kiss him. As a consequence, he finally accepted a surgical approach in the second quadrant, including regenerative periodontal surgery on the self-contained defect between 2.3 and 2.4.
What is regenerative periodontal surgery?
Basic concept
Before describing the actual procedure, it is helpful to explain what regenerative periodontal surgery is. In simple terms, this type of surgery tries to rebuild the tissues that support the teeth. These tissues include:
- The gum
- The alveolar bone
- The root cementum
- The periodontal ligament
Instead of cutting away tissue only, regenerative periodontal surgery uses bone regeneration and biomaterials to form new supporting structures around the tooth.
Self-contained defects and bone regeneration
A self-contained defect is a bone defect surrounded by bony walls. Because the defect is “closed” by bone, it can hold a graft and a blood clot more easily. Therefore, this type of defect is very suitable for regenerative techniques.
When we combine regenerative periodontal surgery, bone regeneration and good plaque control, we can often stabilise or even reverse severe bone loss in selected sites.
Phase 3: regenerative periodontal surgery in the 2.3–2.4 area
Surgical planning and sedation
Once the patient agreed, we planned Phase 3 periodontal treatment, which included regenerative periodontal surgery. The main goals were to:
- Access and clean the deep defect.
- Regenerate bone in the self-contained defect between 2.3 and 2.4.
- Reduce pocket depth and improve prognosis for these teeth.
Because he was very anxious, we decided to use conscious sedation, in addition to local anaesthesia. In this way, he could stay more relaxed throughout the procedure.
Surgical steps
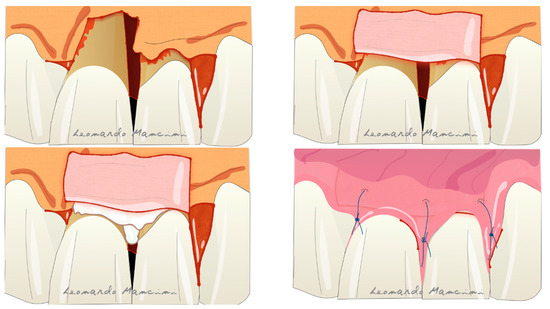
The regenerative periodontal surgery followed these steps:
- Flap design
An intrasulcular incision was made from 2.2 to 2.7. Then, a periosteal releasing incision on the buccal flap provided better access and elasticity. - Debridement and root cleaning
Granulation tissue was removed with scalers and curettes. Next, the root surfaces were carefully planed, and the bone was contoured with specific burs to create a suitable shape. - Bone regeneration in the self-contained defect
The deep defect between 2.3 and 2.4 was self-contained. Consequently, it was ideal for bone regeneration. We filled it with Bio-Oss® and enamel matrix proteins, following a guided tissue regeneration protocol. - Flap closure and occlusal adjustment
After confirming the graft was stable, we sutured the flap with 4-0 sutures. We then checked the bite. The upper left canine had an excessive contact, so we adjusted it to reduce occlusal trauma and protect the regenerated area.
The patient refused orthodontic or orthognathic options for his anterior open bite. Even so, he understood that surgery in this local area was essential to keep those teeth.
Postoperative care and short-term follow-up
Medications and hygiene
After regenerative periodontal surgery, we prescribed:
- Amoxicillin 500 mg for five days.
- Dexketoprofen 25 mg three times a day as anti-inflammatory.
- Chlorhexidine 0.12% mouthwash twice daily for two weeks.
We also instructed him to use a soft toothbrush in the surgical area and to avoid mechanical trauma. Constant reinforcement of hygiene instructions was necessary, because good plaque control is vital for bone regeneration.
Control visits
Sutures were removed after two weeks. In addition, the patient was reviewed weekly during the first month and again at three months. During these visits, we checked healing, reinforced instructions and removed plaque where necessary.
The initial healing was satisfactory, and the patient reported less discomfort and no more pus in the area.
Periodontal re-evaluation and prognosis after regenerative surgery
Results in the treated quadrant
At the next periodontal re-evaluation, the second quadrant showed a clear improvement. Importantly, there were no periodontal pockets deeper than 4 mm with bleeding on probing in the treated area.
Because the surgery was regenerative, we decided not to probe the site aggressively until at least six months had passed. Nevertheless, clinical signs already suggested a stable result.
Therefore, the prognosis of teeth 2.3 and 2.4 changed from uncertain to good, at least in the short term.
Situation in the other quadrants
In contrast, the other quadrants still had deep pockets in teeth such as 3.6, 4.7, 1.5 and 1.6. The patient continued to refuse further surgery in those areas and only accepted scaling and root planing.
As a result, the prognosis of some molars remained uncertain or even poor, especially in the lower left quadrant.
Phase 4: supportive periodontal care and long-term outlook
Maintenance programme
Finally, we moved to Phase 4, also called supportive periodontal care. The objective of this phase is to maintain periodontal stability through regular visits.
During these visits, we:
- Review risk factors such as smoking, alcohol and stress.
- Check plaque levels and bleeding.
- Measure pocket depths where indicated.
- Take X-rays if new symptoms appear.
- Perform targeted scaling and polishing.
If the periodontitis stays under control and there are no deep pockets with bleeding, the interval between visits can be extended. For example, we might see the patient every four months in the first year and every six months in the second year, depending on his cooperation.
Lessons from this regenerative periodontal surgery case
In summary, this case shows several important points:
- Regenerative periodontal surgery with bone regeneration can improve prognosis in sites with self-contained defects, even in complex patients.
- Motivation and communication are just as important as instruments and biomaterials.
- Without surgery, some deep defects do not improve, no matter how many cleanings are done.
- Supportive periodontal treatment is essential to protect the results and slow down the disease in other areas.
Periodontal treatment and bone regeneration at Facialia
At Facialia, in Silla (Valencia), we offer complete periodontal treatment, from basic cleanings to advanced regenerative periodontal surgery and bone regeneration. We also work with anxious or “difficult” patients, adapting sessions and using options like conscious sedation when needed.
If you have bleeding gums, bad taste, loose teeth or have been told you have deep pockets, we can study your case in detail and explain your options in clear language.
You can contact us through Facialia.com or visit us in Silla, Valencia, to see how modern periodontal treatment can help you keep your teeth for many more years.


