Frenectomy, connective tissue graft, sensibility, Miller class 3 gingival recession.
Previous information
Referral
The patient attended the Pontificia Javeriana University (Bogotá, Colombia).
Patient Complaint
«I have sensitivity when it comes to drinking something cold, and I have noticed that the gum retracts more and more.»
History of presenting complaint: The patient attends the university clinic to have a dental filling. After the review, his general doctor referred him to the Master of Periodontics to treat his periodontal health and perform treatments.
Social history
Age: 39 years old
Occupation: Sciences teacher.
Medical history
Actual diseases: Active Periodontitis (Caton et al., 2018) and type 2 diabetes are currently under control.
Allergies: Clavulanic acid.
Tabaco history: Occasionally, five per week.
Alcohol intake: He has problems with alcohol, goes to therapy, and recognizes that he takes at least one bottle of brandy weekly.
Family conditions: Alcoholism and drug addiction, his mother abandoned him when he was little, and he grew up in an orphanage. He knows nothing of his father.
Dental history
Oral hygiene technique: inadequate.
Dental visits: Infrequent.
Habits: He tends to chew on pens, knows this is bad, and breaks his teeth.
Evaluation:
1. Health
2. Function
3. Aesthetics
The maximum aperture was 40 mm in the anterior zone.
Treatments performed before mucogingival surgery
- Cleaning and applying airflow are carried out.
- Radiological diagnostic method: Periapical radiographs and orthopantomography. A CBCT(Leonardi Dutra et al., 2016) was performed when even better image detail was needed to assess periodontal health.
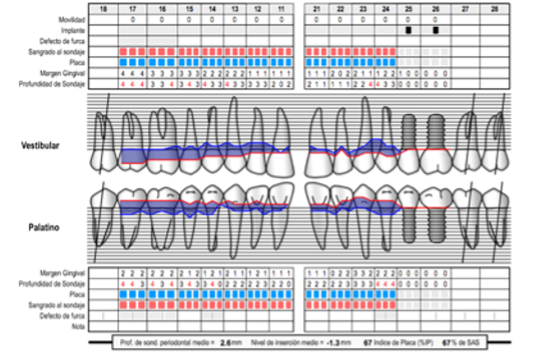
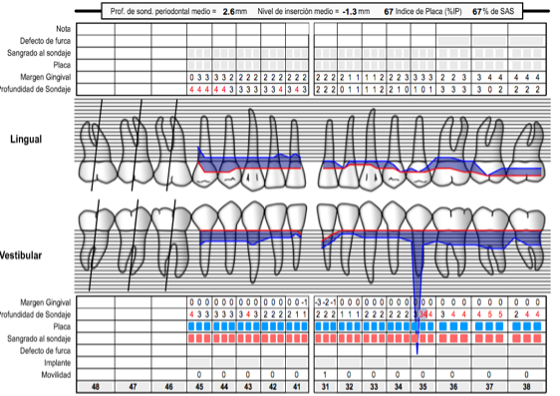
- Perio chart shows the deep pockets and soft tissue conditions:
- CAL generalized were 4 mm in molars and 2 mm in anterior teeth.
- Bleeding and plaque generalized.
- Thin biotype.
- Generalized gingival recessions in superior anterior teeth. The recessions were miller type 1 from 3-4 mm in the anterior teeth, and 2.1 and 1.1 have sensibility.
- Moderate periodontitis(Caton et al., 2018) localized, stadium two and grade two B, Beca, us in the HBA1C glucose test, which the patient had performed two weeks before attending the consultation, its values were £7%. (Baeza et al., 2020)
- The CPITN code was 2 for the majority of her teeth.
Perio chart
Upper:
Lower:
- The patient was taught the instructions and good brushing and flossing techniques. An electric toothbrush is recommended since, according to Ccahuana-Vasquez et al.2019 (Ccahuana-Vasquez et al., 2019), it reduces the level of plaque and gingivitis compared to the manual toothbrush.
- To control plaque levels in the patients, it was recommended to use some tablets to detect plaque after brushing. Thus, they would know if the plaque is being removed and where they need to brush better.
- Scaling and root planning were performed. The aims of this treatment are:
- To reduce bleeding and the level of plaque to £25%.
- To reduce the depth level of the pocket to under 5 mm.
- Keep the horizontal defect less than 2-3 mm in the furcation involved.
- To prevent pain or bad smell.
- To evaluate other techniques, such as regenerative or resective surgery, if this treatment is unsuccessful in the periodontal revaluation carried out after four months.
- The patient was taught about motivation and education about the harmful effects of tobacco and alcohol on health. It was recommended to visit pages such as the Slutta.no page, created by Helsenorge.no, for more information on quitting smoking. In addition, pinto-Filho et al. 2018(Pinto-Filho et al., 2018) conducted a cross-sectional study about alcohol and tooth loss. They found that Alcohol dependence increased 2.5 times the risk of tooth loss.
- Sistematic revaluation was recommended after four months to recheck the periodontal evolution.
Attitudes towards previous treatment
Good attitude.
Systematic facial examination
The face:
Mixed race with Dolichofacial features.
Mouth:
1. Sufficient saliva and good mobility of the tongue.
2. The oral mucosa is moistened, has an average colour and does not present pathologies.
Diagnosis
1.The patient presented Miller recessions(Pini-Prato, 2011) type 3 in 3.1.
2. Moderate Periodontitis, stadium two and grade B in active phase related to Diabetes(Iacopino, 2001).
Differential fixed treatments
1. Use as a connective tissue graft, products such as Alloderm or Mucoderm(Schmitt et al., 2016) have been shown to work in this type of retraction.
2. Make gingival fillings to treat sensibility.
It is ruled out because we would not prevent recessions from continuing to escalate.
3. Perform a free gum graft(Barootchi et al., 2020) and at the same time remove the frenulum.
Wait two months and make a connective tissue graft with a coronal positioning flap.
Treatment
- A connective tissue graft was made in an envelope (Bhatavadekar, Gharpure and Chambrone, 2019).
- A 3.2 to 4.1 incision was made. Said incision was partial-thickness up to the apex of the teeth. The periosteum was used to detach the fibres of the frenulum from the bone and make its insertion more apical.
- The graft was sutured, and a soft diet was recommended for three weeks, nothing of warm drinks, acidic or very salty things.
- Rinses with 0.12% chlorhexidine are recommended from the second day until completing one week.
- Brushing the graft area was prohibited until after three weeks.
- The hygiene kit would have pieces of cotton soaked in salty water.
- The crowns of implants 2.5 and 2.6 were performed four months after implant placement.
Options
Conveniences:
- A palatal connective tissue graft is a widely studied technique supported by the literature (Eren et al., 2016; Cairo, 2017; Bhatavadekar, Gharpure and Chambrone, 2019; Zucchelli et al., 2020).
- In this way, the recession will be prevented from advancing, it will stop, and the patient’s measures will be instilled so that the recession does not reappear.
- Taking the connective tissue graft from the tuberosity decreases the possibility of cutting the palatal artery, making it one more minor complication to worry about.
The connective tissue graft of the tuberosity has more keratinocytes than the palate; it is excellent for achieving volume, although it is less aesthetic than the palate( Sanz-Martín et al., 2019).
Inconveniences:
- It requires more manual dexterity than performing just a gingival filling.
- Necrosis of the tuberosity bone may occur, and the pain may be quite noticeable.(Aguirre-Zorzano et al., 2017)
- It may be that if there is any failure in the suture and placement of the graft, it is lost, and the recession increases. The area could be painful or the donor site(Chiu et al., 2020).

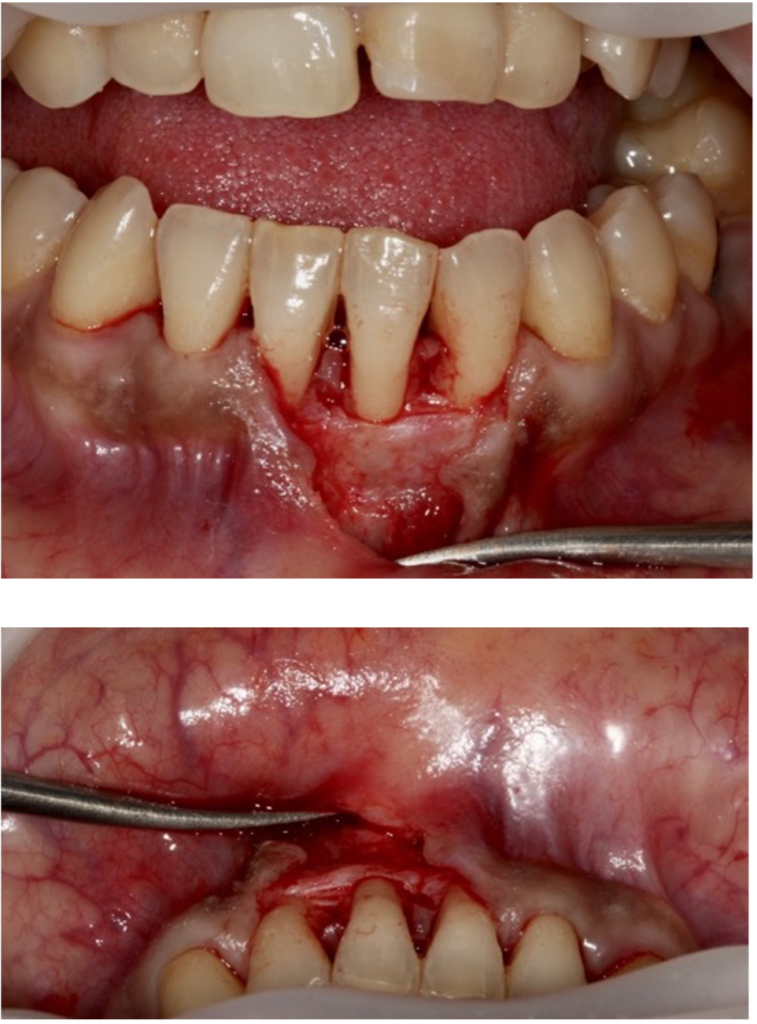
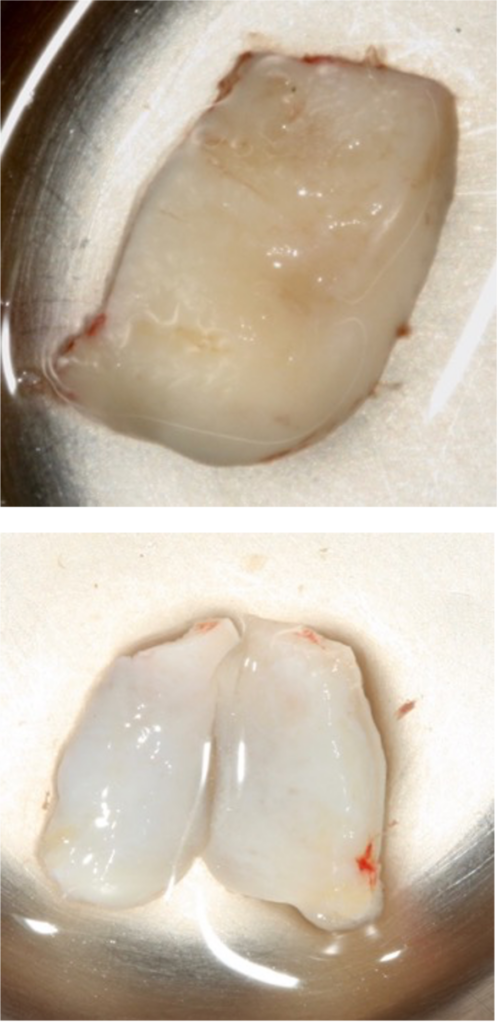
The tuberosity graft was de-epithelialized and divided into two parts without being separated. The vestibular flap would cover one piece, and the other part would be without being covered with the flap. Both factors would remain united.

Baseline Vs post-treatment:

Evolution and prognosis
The evolution and prognosis are good since the insertion of the frenulum, which was the leading cause of the recession of 3.1, has been lowered more towards the apical.
By increasing the volume of the gums, the tooth will be more protected against the next recession.
This graft will evolve favourably.
Overall
In this case, I learned that the frenulum could not only be removed from the buccal with a zetaplasty or with parallel or oval incisions; disinsertion of the fibres from within the flap is a possibility(Sculean and Allen, 2018).
This treatment was made because the recession was minor. However, if it becomes enormous, a total frenectomy must be performed, and in many cases, the chin muscle must be removed to avoid the recurrence of the retraction.



