Introduction
At facialia.com, we offer a comprehensive, multidisciplinary approach to complex dental cases. This case report details the treatment of a 26‐year‐old patient originally seen in a private clinic in Sarpsborg, Norway. She presented with a pronounced Gummy Smile and Gingival Hyperplasia that significantly affected her smile aesthetics. Referred by her orthodontist for wisdom tooth extraction and periodontal treatment, she battled biofilm‐induced gingivitis—exacerbated by metal brackets and poor oral hygiene. Her orthodontic treatment also contributed to her small teeth appearing even smaller, intensifying her Gummy Smile and Gingival Hyperplasia.
Patient Background and Clinical Examination
During her first consultation at facialia.com, the patient expressed deep concern over her excessive gum display. Her maxillofacial surgeon had noted an underlying bone excess, necessitating surgical correction. Clinical findings included a convex facial profile, lack of lip seal, hypermobile lips, and an anterior open bite. The periodontal exam revealed probing depths of up to 7 mm, an average clinical attachment loss of 3 mm, and a thick gingival biotype. Notably, the gingival margin in teeth with brackets was approximately 4 mm above the cementoenamel junction—a finding consistent with literature on Gummy Smile and Gingival Hyperplasia (Caton et al., 2018; Gursoy et al., 2007).
Social History and Contributing Factors
The patient’s social history contributed to her dental condition. Although she is a non-smoker with regular dental visits, her infrequent use of interdental aids—despite being taught superfloss techniques (Wong & Wade, 1985)—and occasional weekend alcohol consumption (about four glasses of wine per week) worsened her case of Gummy Smile and Gingival Hyperplasia. Additionally, her family history of osteoarthritis and fluid retention provided context for her overall treatment planning (Sacitharan, 2019).
Treatment Protocol at facialia.com
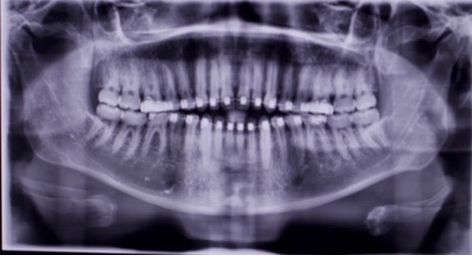
Our treatment protocol at facialia.com is structured in multiple phases. In the first phase, we focused on behavioral change and rigorous biofilm control. The patient received detailed brushing instructions, electric toothbrush recommendations (Ccahuana-Vasquez et al., 2019), and education on the harmful effects of alcohol on periodontal health. This foundational phase aimed to manage her Gummy Smile and Gingival Hyperplasia effectively. Comprehensive scaling and root planing followed, along with radiographs to assess her periodontal status. Despite these measures, persistent inflammation and hyperplasia indicated that her Gummy Smile and Gingival Hyperplasia required further intervention.
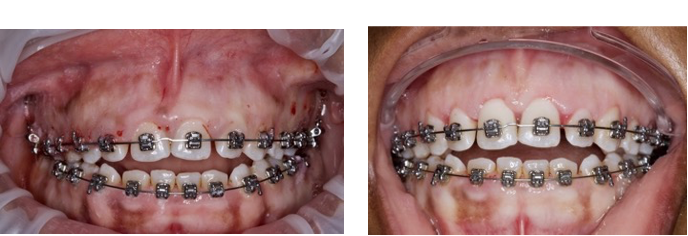
Surgical Intervention: Gingivectomy and Gingival Peeling
The pivotal third phase involved a surgical intervention combining gingivectomy with a gingival peeling procedure. This approach was designed to remove excessive gingival tissue extending from the cementoenamel line to the incisal edge, thereby unveiling proper clinical crown dimensions. The procedure not only enhanced smile aesthetics but also improved oral hygiene and allowed better bracket repositioning. This targeted intervention directly addressed her Gummy Smile and Gingival Hyperplasia. Studies, such as those by Taher et al. (2020) and Dolt et al. (1997), support the effectiveness of these techniques, even when working around orthodontic brackets.
Outcome, Prognosis, and Conclusion
Throughout her treatment at facialia.com, we meticulously planned each step—from reinforcing proper oral hygiene to using adjunctive therapies like chlorhexidine rinses and NSAIDs for postoperative comfort. Although her orthodontic treatment has slowed and her third molars have been extracted, radiographs show that the distance from the bone level to the enamel line has decreased, increasing the apparent clinical crown size. The prognosis for her teeth remains favorable until her planned orthognathic surgery, at which point re-evaluation will be necessary due to potential root resorption or dental mobility. Our comprehensive management of Gummy Smile and Gingival Hyperplasia underscores the strength of our multidisciplinary approach.
O.P.G
Intraoral Photos





Image 1.
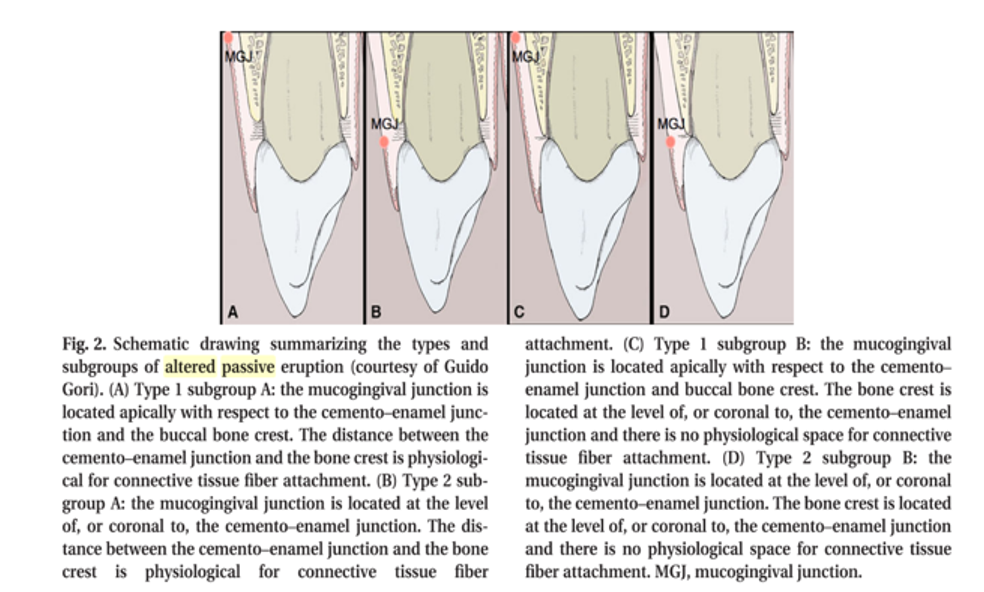
The image is taken from the article by Mele et al. 2018(Mele et al., 2018).
Photos of gingivectomy and peeling for Gummy Smile and Gingival Hyperplasia treatment.
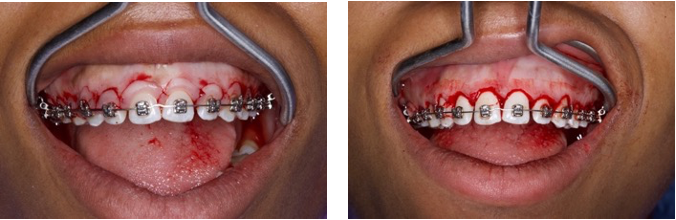
Photo after gingivectomy in the maxilla and starting of the mandible

g the size of the clinical crown(Marzadori et al., 2018).
Periapical X-rays

If you are seeking advanced dental care in Silla, Valencia, visit facialia.com. Our clinic, located at Avenida Reyes Católicos, 3, offers state-of-the-art treatments tailored to your needs. For appointments or inquiries, please call +34 600817409. Discover how facialia.com can transform your smile and overall oral health by expertly treating Gummy Smile and Gingival Hyperplasia.



