Regenerative periodontal surgery, self-contained defect, periodontal treatment, piorrea, enfermedad periodontal, regenerative procedures to save teeth, periodontal disease guided tissue regeneration, understanding periodontal health recognizing the disease, periodontal regenerative procedures to save.
Introduction
At Facialia.com, we believe in preserving your natural teeth through the most advanced periodontal treatments available. This case study showcases how regenerative periodontal surgery helped restore oral health in a patient with severe periodontal disease and self-contained bone defects.
Patient Background
A 46-year-old CEO came to our clinic after more than ten years of periodontal maintenance. He had long-standing periodontal disease, with routine cleanings every five months. Recently, he noticed pus discharge when pressing near the upper left canine, prompting immediate attention.
Medical and Social Overview
- Alcohol Use: 8 glasses of wine per week
- Family History: Diabetes, alcoholism, depression
- Oral Hygiene: Brushing and flossing regularly
- Dental Visits: Frequent
Initial Clinical Assessment
- Generalized periodontal disease, Stage 3 Grade C (Caton et al., 2018)
- Probing depths: 4–5 mm, up to 11 mm interproximal pocket (2.3–2.4)
- Multiple self-contained bone defects
- Miller Class I gingival recessions at 2.3, 2.4, 3.4
- Thin gingival biotype
- Anterior open bite
Phase One: Behavioral Change and Supragingival Control
The focus was on:
- Educating the patient on understanding periodontal health and recognizing disease
- Supragingival plaque removal using airflow
- Motivating proper brushing/flossing and recommending an electric toothbrush
- Using disclosing tablets to visualize plaque
- Counseling on the harmful effects of smoking and alcohol
Phase Two: Subgingival Instrumentation
- Scaling and root planing
- Chlorhexidine irrigation
- Reevaluation after 2 weeks revealed no improvement; a fistula appeared at 2.3–2.4
- Patient finally consented to surgery due to the impact on his relationship and discomfort
Phase Three: Regenerative Periodontal Surgery
What Is Regenerative Periodontal Surgery?
This advanced procedure restores lost bone around teeth. It involves cleaning the infected area and placing regenerative materials like Bio-Oss and Emdogain to stimulate new bone growth.
Surgical Procedure for regenerative periodontal surgery
- Intrasulcular incision from 2.2 to 2.7
- Periosteal release for better access
- Thorough debridement and bone contouring
- Bone grafting with Bio-Oss and Emdogain at the 2.3–2.4 defect
- Sutures placed; occlusal adjustment done to relieve trauma
- Patient refused orthodontic or orthognathic referral
Postoperative Protocol
- Amoxicillin 500 mg x 5 days
- Dexketoprofen 25 mg TID
- Chlorhexidine 0.12% rinses for 2 weeks
- Soft brushing and hygiene reinforcement
- Weekly follow-ups for 1 month; re-evaluation at 3 months
Periodontal Re-evaluation
- Success in second quadrant: No probing done until 6-month maturation
- Remaining quadrants: Persistent deep pockets >5 mm in 3.6, 4.7, 1.5, 1.6
Maintenance Phase (Phase Four)
Ongoing periodontal maintenance is vital:
- Every 3–6 months, based on condition and cooperation
- Full perio charting, mobility and furcation exams
- Scaling, polishing, and restoration checks
- Continuous reinforcement of smoking/alcohol cessation
Tooth Prognosis
- 2.3 and 2.4: Good prognosis after surgery
- 3.6: Poor prognosis, increased mobility
- 4.7, 1.5, 1.6: Uncertain
- Rest of the dentition: Stable
Final Thoughts
This case exemplifies how regenerative periodontal surgery can reverse damage caused by advanced periodontal disease. Self-contained bone defects, when addressed early, can be managed effectively with guided tissue regeneration techniques.
Despite challenges like patient resistance, anxiety, and lifestyle habits, tailored treatment and strong motivation made a meaningful difference. Our team at Facialia.com is committed to preserving your natural teeth whenever possible.
Periapical series
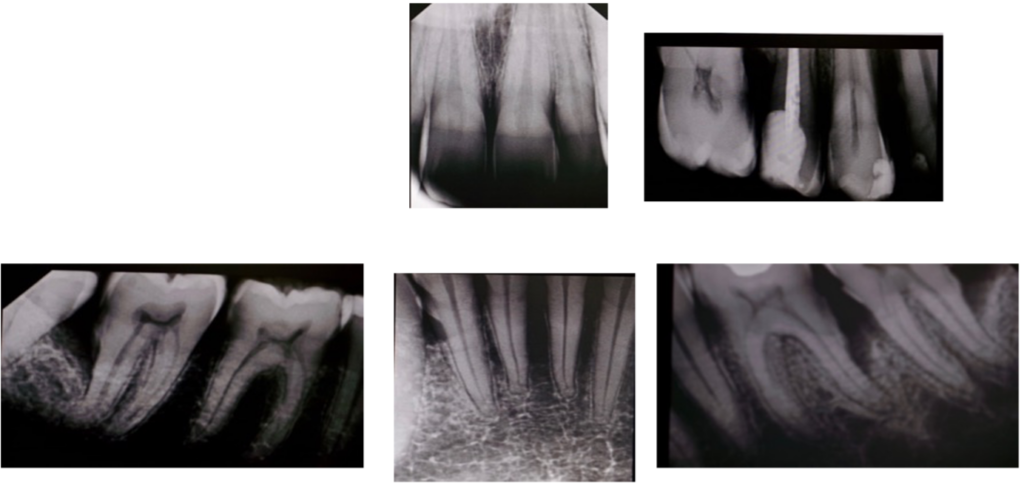
Periapical X-rays
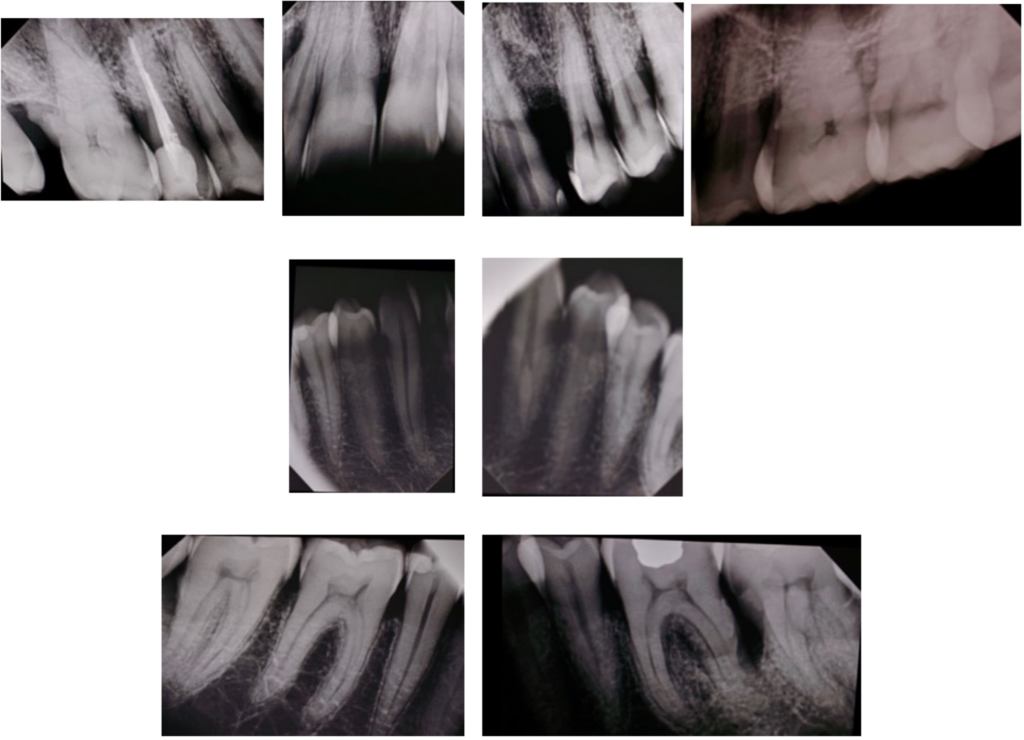
Photo initial

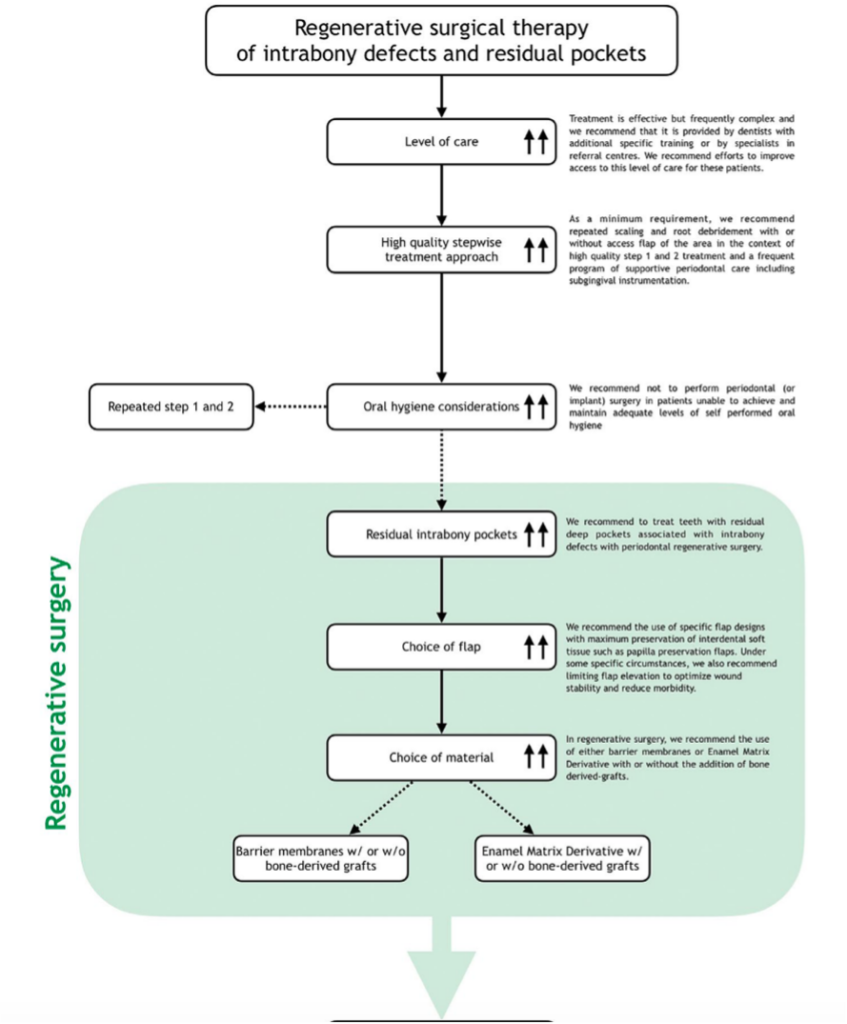
(Sanz et al., 2020)
Surgery photos

Why Choose Facialia.com?
If you’re struggling with gum disease or have been told you might lose teeth, don’t wait. Our specialists are experts in regenerative periodontal therapy. Book your consultation today and discover the path to stronger, healthier gums.




