Chronic discoid lupus erythematosus, whitish lesion on the cheek, periodontitis, enfermedad periodontal y lupus, chronic cutaneous lupus, the scalp.
Previous information
Patient Complaint
« The patient attends an emergency consultation because she has a sharp pain in tooth 1.4.»
History of presenting complaints
In the upper jaw:
1. A vertical root fracture at the level of 1.4 is observed.
2. Regarding her wisdom teeth, they present cavities and an extruded position contact with the jugal mucosa.
3. The restorations, in general, needed improvement.
In the mandible:
1. There is a Periapical lesion of the root of 4.4 and a wisdom tooth included at the 4.8 level.
2. The patient presents a localized bone loss associated with a chronic periodontitis disease.
Personal information
Age: 67 years old
Married: 30 years.
Occupation: Retirement.
Medical history
Current diseases: The patient has hypercholesterolemia controlled with simvastatin (Magán-Fernández et al., 2014).
Allergies: None.
Family conditions: The common disease in her family is Rheumatoid arthritis(Wen et al., 2019). Her mother died of colon cancer, and her Father had a heart attack.
Smoking history: She has not smoked for ten years.
Alcohol intake: Drinks a glass of wine every day.
Dental history
Oral hygiene technique: Inadequate.
Dental visits: The last time was one year ago.
Evaluation:
1. Health
2. Function
3. Aesthetics
The maximum aperture was 40 mm in the anterior zone.
Attitudes Towards Previous Treatment
I pleased the patient and was very involved. She did not think her oral health was compromised, but when she saw the photos, x-rays and other tests, she understood she should follow an oral treatment.
Systematic orofacial examination
1. Dolichofacial patient with solid chewing muscles and limited opening of white skin.
2. The Patient has a solid and prominent tongue.
3. She has good saliva production, the mucous membranes look healthy, and it does not present any lesions on the tongue or oral cavity except the white lesion in the left quadrant.
Diagnosis
A. Gingival recessions in the lingual side of anterior mandibular teeth. The recession Miller type 1 from 1-2 mm.
B. Buccal gingival recessions, 2 mm, Miller type 1 (Pini-Prato, 2011) recession, such as in teeth 1.3, 2.3, 4.3.
C. Degree mobility in teeth 2.8 and 1.8 were 2-3, and CPITN code is 4.
D. Initial periodontitis(Caton et al., 2018) localized in molars, stadium two and grade A.
E. The patient has a well-defined white lesion at the level of the left cheek, at the level of contact between the upper and lower posterior molars (chronic discoid lupus erythematosus manifestation).
F. tooth decay and mobility grade 2-3 (Aminoshariae et al., 2020) at the 1.8 level; 2.8 and 3.8.
G. Condensing osteitis at 4.4 level, this tooth presents a shallow reabsorption root of the root, and the tooth has a negative vitality.
H. Poorly fitting seals that need to be replaced.
I. Vertical fracture from occlusal to apical at the 1.4 level.
Differential Diagnosis
Leucoplakia:
1. Reticular lichen planus: Lichen planus has a bilateral white form of striae (Wickham). In this case, it is unilateral.
2. Acute pseudomembranous candidiasis: White plaques that are mechanically removed and leave bleeding surfaces.
They cannot be detached in this pathology and do not leave bleeding areas.
3. Spongy White Nevus: A bilateral lesion, dense, hairy, white, generalized opacification. It can affect other membranes; the woman has a well-defined and unique white spot that is not removable and has no hair.
4. Leukoedema: whitish opacity on both inner cheeks. It affects mainly patients of African origin. It disappears when the cheek is relaxed. However, In this case, the patient is not black nor has a bilateral injury.
5.Condensing osteitis
6. Idiopathic osteosclerosis.
7. Chronic discoid lupus erythematosus.
Differential Treatment for Leukoplakia
A. Local removal
1. Photodynamic.
2. Therapy laser.
3. Cryotherapy.
B. No removal of the lesion (Holmstrup and Dabelsteen, 2016).
Treatment
Leukoplakia:
1. No treatment; external treatment factors that help mucosal irritation to occur.
2. Conventional removal by scalpel (Holmstrup and Dabelsteen, 2016)if there is no improvement in the clinical aspect of the lesion in three months.
Treatments
Phase one
1. The first step in therapy is to guide behaviour change by successfully motivating the patient to remove supragingival dental biofilm and risk factor control (alcohol and cigarettes, mainly)(Sanz et al., 2020).
To achieve this first step, it is necessary to do the following:
• Supragingival dental biofilm control and develop skills in dental biofilm removal.
Biofilm control

• Interventions to improve the effectiveness of oral hygiene motivation and instructions.
• Adjunctive therapies for gingival inflammation.
• Interventions aimed at removing supragingival plaque and calculus, as well as possible plaque-retentive factors that impair oral hygiene practices.
• Risk factor control includes all the behavioural health change interventions eliminating/mitigating the recognized risk factors for periodontitis onset and progression (smoking cessation, improved metabolic control of diabetes, and dietary counselling and weight loss).
I reevaluated the patient after four weeks to continue building motivation and adherence or exploring other alternatives to overcome the barriers.
1. Cleaning and applying airflow are carried out.
2. Radiological diagnostic method: Periapical radiographs and orthopantomography; CBCT (Aparicio, 2011) was performed to assess periodontal health if necessary.

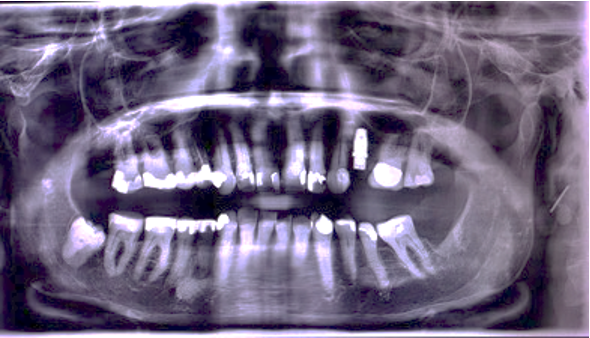
O.P.G. of first check-up
Periapical X-rays:
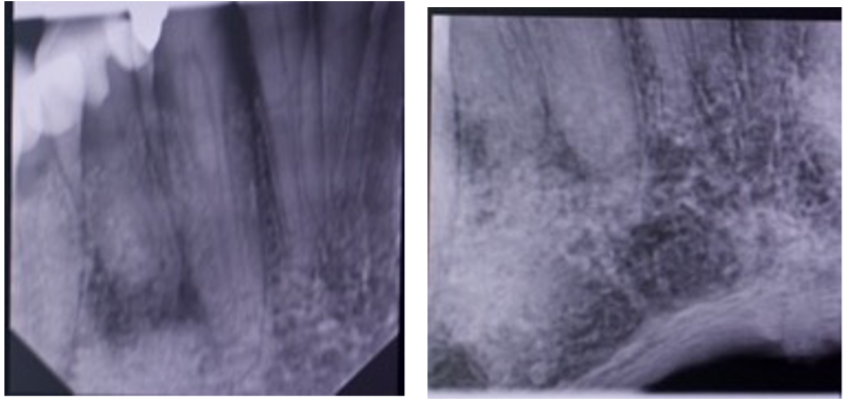
Periapical of tooth 4.4
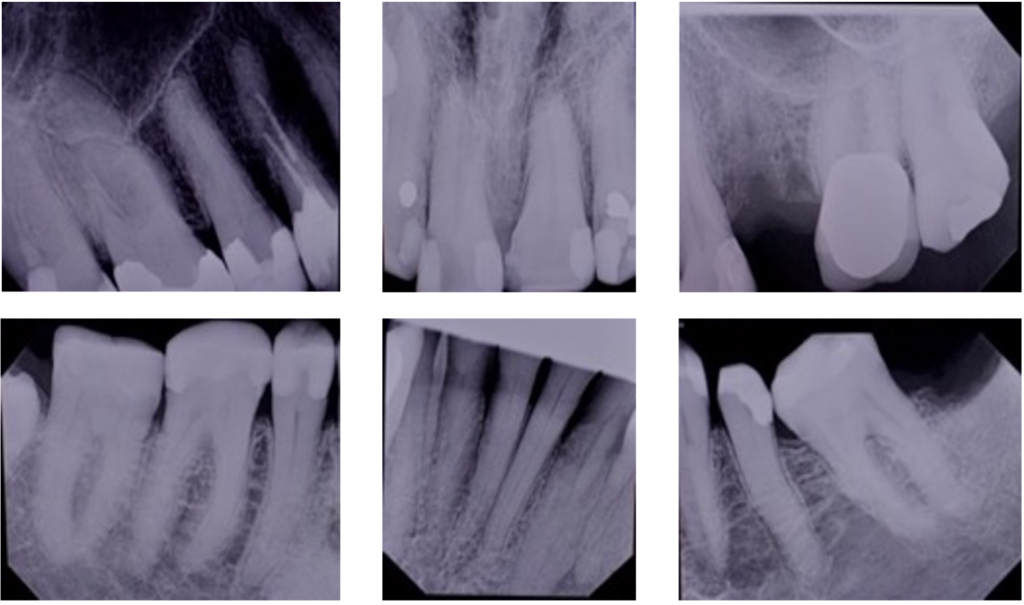
Periapical series
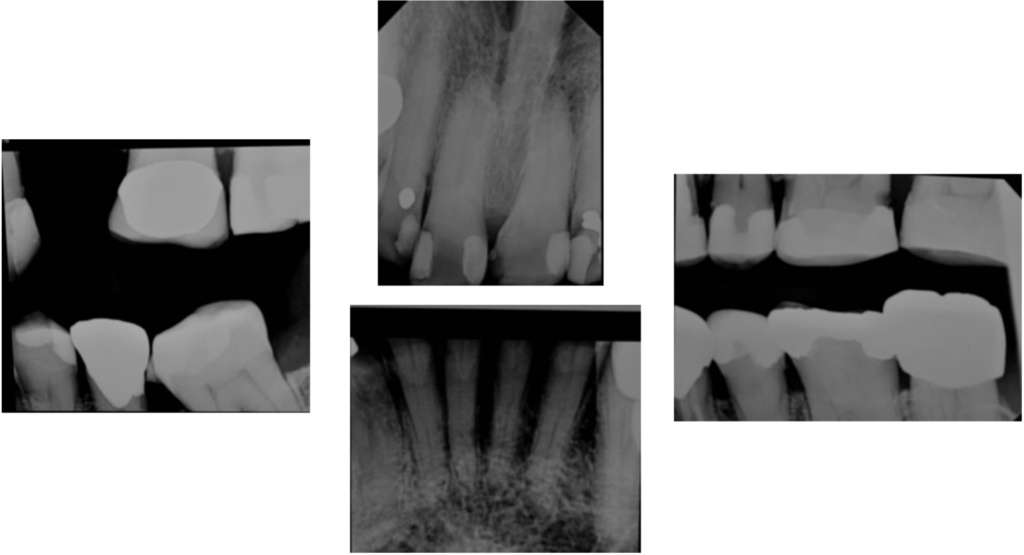
Periapical series
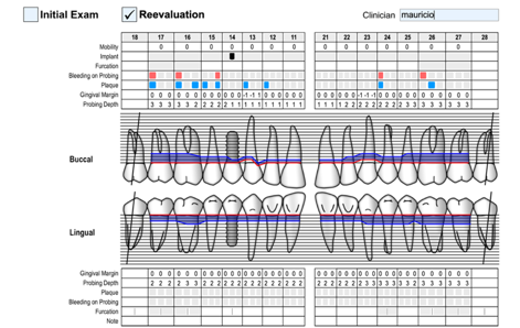
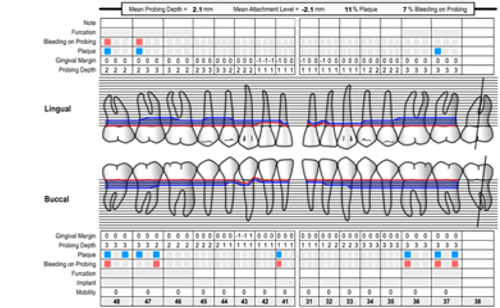
3. Perio chart shows the deep pockets and soft tissue conditions:
A. C.A.L. generalized were 3 mm in molars and 2 mm in anterior teeth.
B. Bleeding and plaque generalized.
C. Thin biotype.
D. Gingival recessions in the lingual side of anterior mandibular teeth. The recessions were Miller type 1 from 1-2 mm.
E. Buccal gingival recessions, 2 mm, Miller type 1 (Pini-Prato, 2011) recession, such as in teeth 1.3, 2.3, 4.3.
F. Degree mobility in teeth 2.8 and 1.8 were 2-3, and CPITN code is 4.
G. Initial periodontitis (Caton et al., 2018) localized in molars, stadium two and grade A.
E. The CPITN code was 2 for the majority of her teeth.
4. The patient was taught good brushing and flossing techniques.
An electric toothbrush is recommended since, according to Ccahuana-Vasquez et al.2019 (Ccahuana-Vasquez et al., 2019), it reduces plaque and gingivitis compared to a regular toothbrush.
As there are tablets to detect plaque after brushing, the patient can know if the plaque is being removed well or where she needs to improve her technique.
5. Scaling and root planning were diagnosed, and this treatment retreatment aimed to reduce bleeding and plaque levels to less than 25%.
A. To reduce the depth level of the pocket to under 5 mm.
B. keep the horizontal defect under 2-3 mm in the furcation involved.
C. To prevent pain or bad smell.
D. To evaluate other techniques, such as regenerative or resective surgery or re-scaling, if this Treatment is unsuccessful in the periodontal revaluation carried out after four months.
6. The patient was educated on the harmful effects of tobacco and alcohol on health. Visiting pages such as Slutta.no by Helsenorge.no were suggested for more information on how to stop smoking and drinking. In addition, Pinto-Filho et al.2018, conducted a cross-sectional study about alcohol and tooth loss.
They found that Alcohol dependence increased 2.5 times the risk of tooth loss.
To control plaque levels in the patients, it was recommended to use some tablets to detect plaque after brushing. Thus, they would know if the plaque is being removed and where they need to brush better.
Phase two
The second therapy step aims to control (reduce/eliminate) the subgingival biofilm and calculus (subgingival instrumentation). In addition to this, the following interventions may be included:
• Use of adjunctive physical or chemical agents
• Use of adjunctive host-modulating agents (local or systemic)
• Use of adjunctive subgingival locally delivered antimicrobials
• Use of adjunctive systemic antimicrobials (Sanz et al., 2020)
1. Scaling and root planning were performed. Irrigated with 0.12% chlorhexidine and hydrogen peroxide.
In addition, a broad-spectrum antibiotic will be prescribed to fight bacteria, like Amoxicillin 250 mg three times per day for five days and metronidazole 500 mg three times daily for five days.
This treatment aims:
A. To reduce bleeding and plaque levels to 25%.
B. To reduce the depth level of the pocket under 4 mm plus B.O.P. and any P.P.D. 6 mm.
C. Keep the horizontal defect less than 2-3 mm in the furcation involved.
D. To prevent pain or bad smell.
E. To evaluate other techniques such as regenerative or resective surgery or re-scaling and root planning again if this Treatment is unsuccessful in the periodontal revaluation carried out after six weeks.
Wisdom teeth: Extraction of 1.8, 2.8, and 2.4.
Condensing osteitis and apical lesion of 4.4: The Treatment was to do an endodontic treatment of 4.4 and wait for evolution. Eliasson et al. 1984 (Eliasson, Halvarsson and Ljungheimer, 1984) reported a study where they validated this procedure.
The maladaptive fillings would be changed, and tooth 1.4 would be removed. It would wait two months, and a dental implant would be placed when the periodontal disease was stabilized.
Tooth 1.4: Extraction and, after three months, it will be placed a dental implant.Photos after teeth extractions
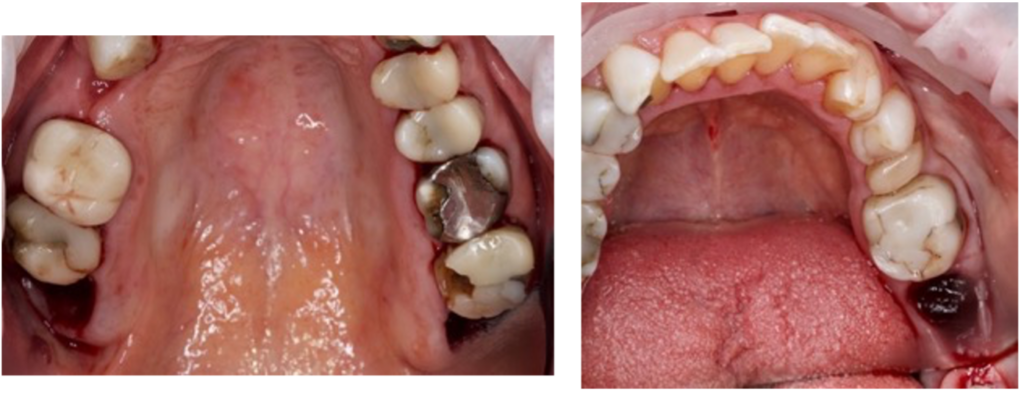
Photos after teeth extractions
2. Options for Treatment of the white lesion
In this case, treating the white lesion eliminated the factors that irritate the mucosa. If, after two months, this lesion grows or presents symptoms, an excisional biopsy will be performed.
- The convenience: Conservative Treatment: Treatment will be done if it does not work.
- The inconvenience: We are not doing an excisional biopsy. We could be skipping an essential step since leukoplakia is a premalignant lesion. However, when it is well-defined, it has a low malignancy index.
Regarding condensing osteitis, the treatment was endodontic treatment.
- The convenience of this option is that it is not an aggressive treatment, which only affects tooth 4.4.
- The downside could be that it did not work and that the tooth had to be extracted.
Photo of the white lesion and broken tooth 2.4
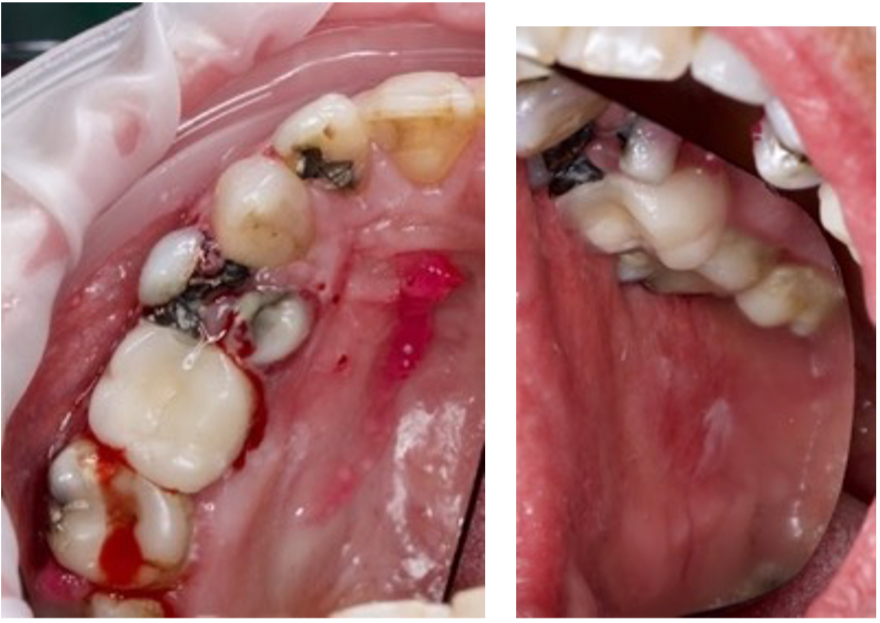
Photos of the white lesion

Surgery/Treatment details
- To polish the restorations of the posterior teeth. The patient was referred after three weeks, and it was verified that there had been no improvement in the lesion.
- Clotrimazole is prescribed 10 mg troches, and a 14-day course of five tablets a day is prescribed (Holmstrup and Dabelsteen, 2016) since it was sought that if the lesion were a lichen planus, it would not be infected with a yeast infection (Hellstein and Marek, 2019).
- After 14 days, the patient was reviewed, and no significant improvements were observed. It was seen that the wisdom teeth continued to cause trauma, and it was decided to remove them.
- It was the extraction of the erupted wisdom teeth.
- Antibiotic therapy was prescribed: amoxicillin 500 mg 1 every 8 hours for seven days. It was cited for control.
- Regarding 44, endodontics will be performed.
- The patient was motivated and educated about the harmful effects of tobacco and alcohol on health.
It was recommended to visit pages such as the Slutta.no page, created by Helsenorge.no, for more information on quitting smoking. In addition, pinto-Filho et al. 2018 (Pinto-Filho et al., 2018) conducted a cross-sectional study about alcohol and tooth loss.
They found that Alcohol dependence increased 2.5 times the risk of tooth loss.
Re-evaluation
After scaling and root planning, the sensation of bleeding and plaque improved. The aims of therapy were achieved:
- No periodontal pockets >4 mm with bleeding on probing or no deep periodontal pockets ≥6 mm.
- No pain in 1.4.
The third step of therapy should be considered. Some specific situations follow directly to phase three, such as tooth mobility with no antagonist.
Prognosis per teeth (Mcguire 1991)
If the treatment does not achieve the therapy endpoints, the patient should not be placed in supportive periodontal care (S.P.C.) programme (Herrera et al., 2022). In this case, this patient, after phase two, was established in phase four.
The prognosis is generally uncertain due to her dental plaque buildup, the position of her teeth, and the non-dissolving white patch that appears on the left and right sides of her cheeks.
It has already been explained that teeth 2.4, 2.8, and 1.8 were extracted.
The individual prognosis is good since their teeth have retained much interproximal bone, taking into account their poor hygiene before starting this treatment.
The patient had good hygiene, plaque levels less than 30%, and periodontal pockets less than 4 mm. Phase 4 of the Treatment will be started.
Supportive periodontal care
It aims to maintain periodontal stability in all treated periodontitis patients by combining preventive and therapeutic interventions to define therapy’s first and second steps, depending on the gingival and periodontal status of the patient’s dentition.
This step should be rendered regularly according to the patient’s needs (Herrera et al., 2022).
Patients may need retreatment if the recurrent disease is detected in any of these recall visits. In these situations, a proper diagnosis and treatment plan should be reinstituted.
In addition, compliance with the recommended oral hygiene regimens and healthy lifestyles are part of supportive periodontal care. Finally, tooth extraction may be considered in any therapy step if the affected teeth have a hopeless prognosis(Sanz et al., 2020).
Throughout the periodontal maintenance phase, a biopsy of the white lesion was performed since it had not reduced in size and had not fully responded to the polishing treatment of the cusps that produced trauma to the cheek.
Once the bone in the area of 2.4 had healed, a Biomed BOPT 4/3 10 mm implant was placed.
Photos of Mucosa before and after biopsy

The biopsy was sent to Oslo Universitetssykehus:
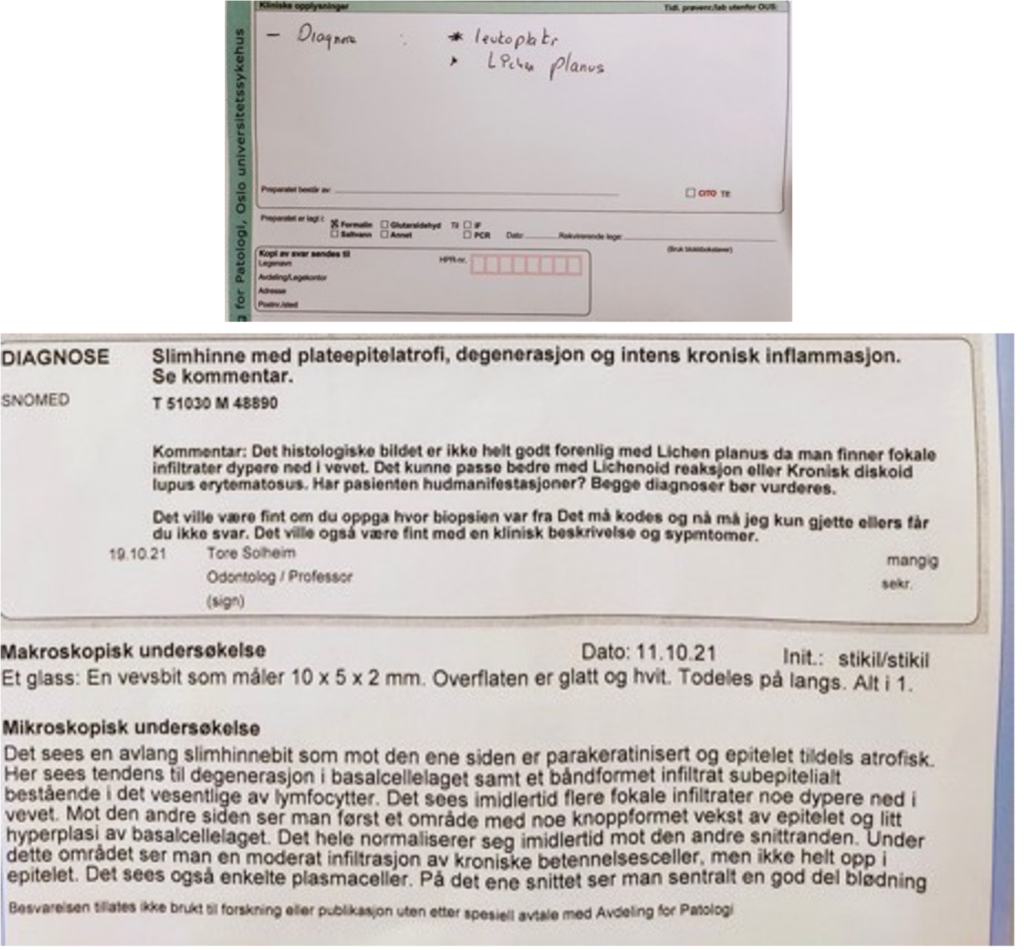
What is chronic discoid lupus erythematosus, and what Treatment for chronic discoid lupus erythematosus?
“Discoid lupus erythematosus (DLE) is a chronic cutaneous disease characterized by inflammatory plaques that may lead to disfiguring scarring and skin atrophy without prompt diagnosis and treatment. However, there is limited evidence for which treatments are most effective. Currently, no medications have been approved specifically for the treatment of DLE. Many of the drugs described in the literature were developed for use in other immune disorders. This review will summarize current therapeutic options for DLE and their supporting evidence with discussion of prevention, topical measures, physical modalities, and systemic therapies, including newer potential therapies” (Garza-Mayers AC, McClurkin M, Smith GP. Review of treatment for discoid lupus erythematosus. Dermatol Ther. 2016 Jul;29(4):274-83).
To perform the periodontal evaluation, the following treatments were performed:
- Periochart; control plaque; cleaning with scaler and airflow.
UP:
DOWN:
Intraoral photography.

Orthopantomography.
Intraoral photo.
The aims of this Treatment
A. To reduce bleeding and the level of plaque to £25%.
B. To obtain a depth pocket level under 4mm.
C. To have no pain or bad smell.
The patient has reduced her plaque and bleeding levels. She is brushing three times daily for one minute and flossing once daily.
At the 1.4 level, there is already enough bone to place the implant, so a punch is made, a Biomed 3i BIOPT 4/3 x 10 implant is placed, and the healing abutment is placed, which serves as a scan body. The patient will be scheduled in six months for periodontal maintenance if necessary.
General prognosis
It is uncertain due to the possibility that the patient has lupus erythematosus. However, she feels fine, has no symptoms, nothing hurts, and she follows the doctor’s instructions. Therefore, an attempt has been made to carry out a conservative treatment.
Regarding the white lesion that the patient has, predisposing factors were eliminated, such as trauma from cheek biting.
However, this did not work so well, and a biopsy was performed to rule out any malignant pathology, although the patient does not present with swollen lymph nodes, does not have pain, and the lesion has not increased in size.
Regarding his periodontal disease, a correct brushing technique and the plaque detector were instilled after it.
Some articles say it is sometimes better not to remove a well-defined oral leucoplakia, as Holmstrup & Dabelsteen in 2016 (Holmstrup and Dabelsteen, 2016).
That is why we wait these months to see evolution, not seeing any improvement. So, it was decided to remove it.
After the biopsy result, the patient was asked to complete a check-up by an endocrinologist and request a study to rule out lupus erythematosus. This study revealed that the patient had chronic discoid lupus erythematosus. The patient did not present symptoms, but she immediately began to treat her disease.
Teeth prognosis
- Tooth 4.4: needs root canal treatment; its prognosis will be uncertain. Depending on its Treatment, Treatment could go into good or bad prognosis.
- Tooth 2.7: needs a new reconstruction because it is leaking. Its prognosis will be good if it does not need endodontic Treatment. However, if it needs rot treatment, its forecast would be bad since root canals are calcified.
- The rest of the teeth have a good prognosis, considering their periodontal status and the patient’s age.
Re-evaluation
The patient attends the consultation every four months for a maintenance phase during the first eight months of 2022.
During this time, scaling and root planning are performed at some points of the lower anterior incisors and in the molar area. Generalized cleaning and the patient is motivated through plaque controls to improve their hygiene.
The health remains stable, but the 2.4 implants failed in November 2022. It is decided to wait until April 2023 since her T lymphocyte levels are low, and we should wait for them to rise again. The patient will undergo a new analysis in April 2023.
In her last reassessment, plaque control, periapical series, instruction and motivation on oral hygiene were performed; luckily, she does not smoke and does not drink alcohol currently.
Some metal and composite fillings were polished, the scaler was used in some points of the oral cavity, and the airflow was used.
Regarding the mucosal lesion, it disappears on the left side, but on the right side, it remains stable. It has not grown, and there is no pain or itching.
Mucosa photo right side

General prognosis
Her hygiene has worsened, with widespread plaque. Bleeding in less than 30% of the teeth.
She continues to attend his maintenance consultations and is waiting to have the implant again from 2.4 if his doctor allows us; otherwise, other alternatives will be studied, such as making a ceramic bridge from 23 to 25.
Her general prognosis is uncertain since her health has recently decreased in the last year.
Teeth prognosis
They have a good prognosis; she has no pain, no caries, and the recessions have no symptoms.

