Management of periodontal diseases, generalized aggressive periodontitis, periodontitis gum disease, oral rehabilitation surgery, dental implants and composite veneers.

Introduction
Patients who fear the dentist go to a private dental clinic in Sarpsborg (Norway) for a periodontal assessment. The patient has much complexity because she cannot smile, does not like her teeth, and lacks self-confidence. However, she recently separated and wants to rebuild her life.
History of present complaints
The patient comes to the consultation crying, with a mixture of pain and nervousness. She knows that her teeth are bad, but apart from that, she is terrified of the dentist due to a traumatic experience when she was little.
The patient arrives with a phlegm on the right side of the face, trismus, swelling and general malaise. She tells us that she has not slept well in two nights and is coming today because she cannot take it anymore.
Medical history
The patient presents nodular goitre and takes medication.
She suffers from depression and anxiety; she is under medication.
She smokes 15 to 20 cigarettes a day and does not drink alcohol.
Social history
Age: 37 years old
Occupation: ITI business.
Attitudes Towards Previous Periodontal Disease Treatment
Good attitude, Cooperative patient.
Dental history
Oral hygiene: Brushes her teeth, not floss or superfloss (Wong and Wade, 1985). When she feels pain, she does not clean her teeth.
Dental visits: Frequent.
Evaluation:
1. Health
2. Function
3. Aesthetics
Due to the trismus, the maximum aperture was 29 mm in the anterior zone.
Dental emergency management
After seeing the patient’s nervousness and pain, I first reassured her and asked her if she was allergic to Amoxicillin and Voltaren. She said she was not given 500 mg amoxicillin and 50 mg voltaren doses. Then, she takes them to drink a relaxing infusion.
It was explained to the patient that I could not do anything since she could not open her mouth. The antibiotic and anti-inflammatory treatment duration was indicated, and she was given an appointment the following week to start phase one of the treatment.
Periodontal Treatments (Management of periodontal diseases)
How can periodontal disease be managed?
phase one
1. The first step in therapy is to guide behaviour change by successfully motivating the patient to remove supragingival dental biofilm and risk factor control.
To achieve this first step, it is necessary to do the following:
• Supragingival dental biofilm control and develop skills in dental biofilm removal.
• Interventions to improve the effectiveness of oral hygiene motivation and instructions.
• Adjunctive therapies for gingival inflammation
• Interventions aimed at removing supragingival plaque and calculus, as well as possible plaque-retentive factors that impair oral hygiene practices.
• Risk factor control includes all the behavioural health change interventions eliminating/mitigating the recognised risk factors for periodontitis onset and progression (smoking cessation, improved metabolic control of diabetes, and dietary counselling and weight loss).
I reevaluated the patient after six weeks to continue building motivation and adherence or exploring other alternatives to overcome the barriers.
Management of periodontal diseases
1. Cleaning and applying airflow are carried out.
2. Radiological diagnostic method: Periapical radiographs and orthopantomography.
3. Perio chart shows the deep pockets and soft tissue conditions:
A. CAL generalised were 3-4 mm in molars and 2-3 mm in anterior teeth.
B. Deep pockets were 6 mm in 4.6, 1-2 mm in maxilla teeth and 4-5 mm in mandibular anterior teeth.
C. Bleeding and plaque generalised.
D. Thin biotype.
E. Advanced periodontal disease with the possibility of losing more than one tooth, stage 2 and grade C(Caton et al., 2018).
F. The CPITN code was 3 for the majority of her teeth.
4. The patient was taught the instructions and good brushing and flossing techniques. An electric toothbrush is recommended since, according to Ccahuana-Vasquez et al. (Ccahuana-Vasquez et al., 2019), 2019 reduces plaque and gingivitis compared to the manual toothbrush.
5. To control plaque levels in the patients, it was recommended to use some tablets to detect plaque after brushing. Thus, they would know if the plaque is being removed and where they need to brush better.
6. The patient was taught with motivation and education about the harmful effects of tobacco and alcohol on health. It was recommended to visit pages such as the Slutta.no page, created by Helsenorge.no, for more information on quitting smoking. In addition, pinto-Filho et al. 2018(Pinto-Filho et al., 2018) conducted a cross-sectional study about alcohol and tooth loss. They found that Alcohol dependence increased 2.5 times the risk of tooth loss.
7. Systematic revaluation was recommended after three weeks.
Diagnosis
1. Generalised periodontal disease with the possibility of losing more than one tooth, stage 2 and grade 3(Caton et al., 2018).
2. Presence of vertical fracture in rot 2.5.
3. Abscess with a fistula at the level of 4.6 in an endo-periodontal type lesion; this tooth has mobility grade 3.
4. root pieces in 4.8; 1.7; 3.6; 3.7.
Teeth prognosis (Mac Guire 1991)
Teeth 4.6, 4.8, 2.5, 3.6, 3.7 predict extraction.
The lower incisors have a guarded prognosis. The rest of the teeth have a good prognosis.
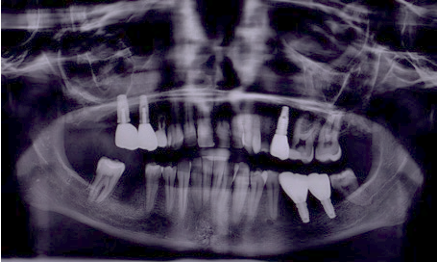
Initial OPG

Initial photo

Once phase one was completed, making the patient understand why her gums were bleeding and the importance of controlling the plaque, we began phase two of the treatment.
Phase two
The second therapy step aims to control (reduce/eliminate) the subgingival biofilm and calculus (subgingival instrumentation). In addition to this, the following interventions may be included:
• Use of adjunctive physical or chemical agents • Use of adjunctive host-modulating agents (local or systemic) • Use of adjunctive subgingival locally delivered antimicrobials • Use of adjunctive systemic antimicrobials(Sanz et al., 2020)
The treatment is based on gaining the patient’s trust; the first appointments are to have contact with her, talk, and start doing the periodontal treatment little by little.
1. Scaling and root planning were performed. The aims of this treatment are:
A. To reduce bleeding and the level of plaque to £25%.
B. To reduce the depth level of the pocket under 4 mm plus BOP and any PPD > 6 mm.
C. Keep the horizontal defect less than 2-3 mm in the furcation involved.
D. To prevent pain or bad smell.
E. To evaluate other techniques such as regenerative or resective surgery or re-scaling and root planning again if this treatment is not successful in the periodontal revaluation carried out after six weeks.
2. The patient was taught with motivation and education about the harmful effects of tobacco and alcohol on health. It was recommended to visit pages such as the Slutta.no page, created by Helsenorge.no, for more information on quitting smoking. Pinto-Filho et al. 2018(Pinto-Filho et al., 2018) conducted a cross-sectional study about alcohol and tooth loss. They found that Alcohol dependence increased 2.5 times the risk of tooth loss.
3. Extraction of the pieces with a lousy prognosis
4.6 for having an endo-periapical abscess with dental mobility.
2.5 for being a radicular rest with a vertical fracture.
3.6: Apical cyst in the mesial root.
3.7 and 4.8 because they are root remains without being restored.
OPG after extractions

Teeth prognosis (Mac Guire 1991)
After scaling, root planning, and the other phase two treatments, the prognosis for the remaining teeth is good. The patient has good hygiene techniques, has learned quickly, floss and has purchased an electric toothbrush. In addition, she knows how to drive very well.
4. Periodontal re-evaluation
The aims of therapy:
No periodontal pockets >4 mm with bleeding on probing or no deep periodontal pockets ≥6 mm.
If this is not done, in that case, the third step of therapy should be considered. Some specific situations follow directly to phase three, such as tooth mobility with no antagonist.
If the treatment successfully achieves the therapy endpoints, patients should be placed in supportive periodontal care (SPC) programme.(Herrera et al., 2022).
1. After scaling and root planning, indicating the brushing and flossing technique to the patient, the patient was summoned for a review two weeks later.
2. The results were favourable; the gingiva was not bloody and did not show gingival hyperplasia.
Once the patient presented optimal periodontal health, without dental mobility greater than grade 2, without a plaque index greater than 15%. Without bleeding on pocket probing greater than 30% of the sites, the patient was ready to move on to the periodontal maintenance phase and start the rest of the treatments.
Phase four
It aims to maintain periodontal stability in all treated periodontitis patients by combining preventive and therapeutic interventions defined in therapy’s first and second steps. It is realised from three to six months after phases one, two or three, depending on the severity of the condition, age, and cooperation.
The must be rechecked risk factors, do the perio chart again.
- Register of dental biofilm.
- PPD.
- Furcations invoice exam.
- Mobility.
- X-rays if there are clinic changes or pain.
Scaling and root planning and polish restorations in specific points:
A. To reduce bleeding and the level of plaque to £25%.
B. To reduce the depth level of the pocket to under 5 mm.
C. Keep the horizontal defect under 2-3 mm in the furcation involved.
D. To prevent pain or bad smell.
If everything is controlled and there are no periodontal pockets >4 mm with bleeding on probing or no deep periodontal pockets ≥6 mm, the control appointment will be the first year every four months and the second year every six months; This must be agreed upon with the patient, his cooperation, and financial conditions.
- (Pinto-Filho et al., 2018) Conducted a cross-sectional study about alcohol and tooth loss. They found that Alcohol dependence increased 2.5 times the risk of tooth loss.
Plan Management of periodontal diseases
- composite veneers and superior smile design are made to improve the patient’s self-esteem:
In this case, the idea was to correct the position of the central incisors and polish the lateral ones so that the aesthetics would look more uniform. Ameloplasty was performed in 2.1 and 1.1 to ensure the teeth were correctly positioned. Once this was achieved, to level the vestibular surface, it was decided in 1.1 to apply a composite veneer. The chosen shade was A.3 vita, mixed with M bleach, both Tetric Evo Ceram composites. Alcohol was involved in cleaning the dental surface. It was left for 20 seconds. Then, it was washed, and 37% orthophosphoric acid was used between 4 and 5 minutes; it was passed, and a layer of adhesive was applied. Finally, I removed the excesses with the air syringe and photo-polymerised them.
- The next step was applying a mixture of the Evo Ceram bleach M and A.3 vita syringe. Next, the composite was placed in layers to separate the teeth’ transparent plastic bands, and in some cases, Teflon was used.
- Once the composites were light-cured, they were polished with a very fine Arkansas bur and diamond bur, designing the contours, the emergence profile, and the incisal inclination.
- The next step was polishing using the polishing discs, from the coarsest to the finest. This polishing process is the longest and usually requires several appointments until the patient is happy with the colour and shape.
Photo after cleaning and the vestibular resins in 2.1 and 1.1

Re-evaluation
The aims of therapy:
No periodontal pockets >4 mm with bleeding on probing or no deep periodontal pockets ≥6 mm.
Once the patient has complied with the above requirements, verified by plaque control, probing depth, sensitivity test and dental mobility, and checking bleeding after examination, The planned treatment plan is continued: the placement of dental implants.
Oral photo control


Dental implants plan
- The dental implants (Biomed 3i BOPT) were placed after the last re-evaluation.
Surgery photo
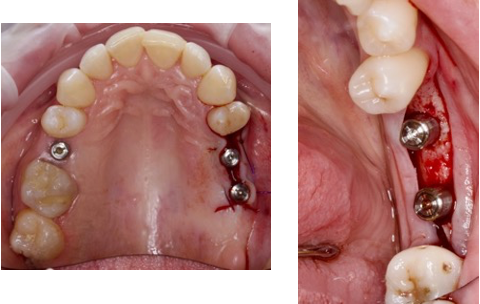
Re-evaluation after the placement of the implants
Four months from the placement of the implants except 4.6, since its radiographic appearance suggested waiting longer to heal the new bone tissue was necessary.
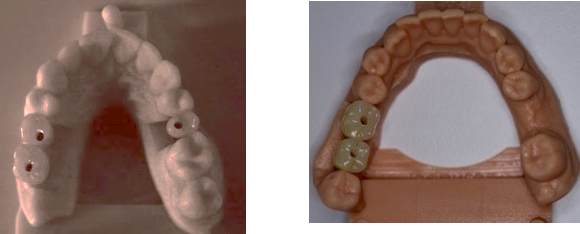
The patient was reviewed and verified that the implants were prepared to be scanned and made their crowns. Four months after the placement of the implants, using the Encode® pillars as healing abutments and scan body, the implants were scanned by iTero® scanner.
Two weeks after the scanner, the crowns are placed at 30 Ncm of torque, and the patient attends a review at two weeks and a month.
The patient must attend a consultation twice a year for control of implants and periodontal maintenance.
OPG implants

Photo with implant placement
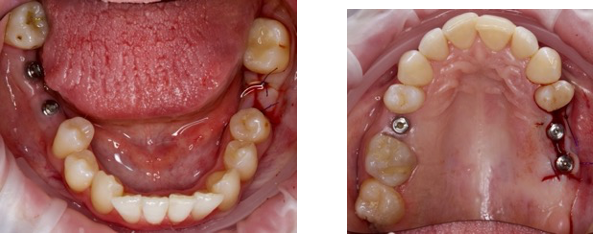
Images from iTero scanner

Digital model
Re-evaluation
Once the treatment has been completed, the patient is scheduled for a weekly and monthly check-up. Occlusion, mobility, interdental space, colour, and relationship with the gum are reviewed.
When these requirements have been met, a check-up every five months is agreed upon with the patient to maintain his periodontal control, where a plaque test, sensitivity, bleeding on probing, and caries check will be done.
Once this is done, cleaning will be done with prophylactic paste and airflow, where it is necessary to use the scaler or curettes.
Intraoral photos

OPG with implants and crowns
Overall
In this patient, we can see a clear example that the results achieved with dedication, hygiene instruction, and brushing techniques are excellent. With the Management of periodontal diseases, She currently has plaque control of less than 10%, he does not have dental discomfort, and she is not afraid to smile.
In this case, the treatment has been quite favourable and enthusiastically accepted by the patient.



