All-on-five, zygoma implants, immediate loading, definitive ceramic prosthesis, bone regeneration.
Referral
A general dentist referred this patient to a dental clinic in Zamora for a fixed solution in this patient.
Patient Complaint
«I cannot use a removable prosthesis. This prosthesis produces pain and injures my mouth. »
History of presenting complaints
The patient has used his removable prostheses for five years. The patient received a bullet in the first quadrant that pierced the bone of the 1.3, 1.4, 1.5, 1.6. Therefore, the maxillofacial surgeon at the Coruña hospital recommended that he wait two years before attempting any regeneration treatment.
Social history
Age: 43 years old
Divorce: 5 years.
Occupation: Bartender.
Medical history:
Actual diseases: The patient is under Treatment with Methadone. He left the drugs two years ago.
Past illnesses: kidney failure, high sugar levels, anxiety, depression.
Allergy: None.
Family conditions: High hypertension.
Alcohol intake: He was an alcoholic and left two years ago.
Tobacco: He smoked 20 cigarettes per day.
Dental history
Oral hygiene technique: Inadequate
Dental visits: Infrequent
Reasons for tooth loss: Periodontal disease, caries, drugs.
Oral pain: He had pain in his anterior teeth; these teeth have mobility grade 2-3(Aminoshariae et al., 2020).
Habits: He does eat a soft diet, nothing complex.
Evaluation:
1. Health
2. Function
3. Aesthetics
The maximum aperture was 42 mm in the anterior zone.
Dental treatments performed before surgery
1. Cleaning and applying airflow are carried out.
2. Perio chart to know the hard and soft tissue conditions:
A. Bleeding and plaque generalized.
B. The patient has gingival recessions Miller type 1(Pini-Prato, 2011)in the mandibular anterior teeth.
C. Gingival biotype thin.
D. Deep pockets in the mandible of 3 mm average in anterior teeth and in posterior was 4 mm.
E. CAL values 3 mm.
F. Radiographic bone loss in the coronal third, 2 mm on average.
3. Scaling and root planning were performed; the aims for this Treatment are:
A. To reduce Bleeding and the level of plaque to £25%.
B. To reduce the depth level of the pocket under 5 mm.
C. Keep the horizontal defect less than 2-3 mm in the furcation involved.
D. To prevent pain or bad smell.
E. To evaluate other techniques such as regenerative or respective surgery if this Treatment is unsuccessful in the periodontal revaluation carried out after four months.
4. The patient was taught about motivation and education about the harmful effects of tobacco and alcohol on her health. It was recommended to visit pages such as the Slutta.no page, created by Helsenorge.no, for more information about stopping smoking. Pinto-Filho et al. 2018(Pinto-Filho et al., 2018) conducted a cross-sectional study about alcohol and tooth loss; they found that Alcohol dependence increased 2.5 times the risk of tooth loss.
5. Sistematic revaluation will be done after four months to check the periodontal conditions.
Attitudes Towards Previous Treatment
Good attitude
Systematic orofacial examination
The face:
Caucasian man with brachyfacial features. The muscles had hyperactivity due to the patients had bruxism(Chrcanovic, Albrektsson and Wennerberg, 2015).
Mouth:
1. Insufficient saliva, a saliva test was performed, and his values were 650 ml(Turner, 2016).
2. Presented tissue lesions due to dry mouth(Wang, Thomson and Craig, 2020). He said his General doctor said it was for the methadone and the effects secondary to the drugs.
Diagnosis
1. Atrophic bone in Maxilla.
2. Mobility of upper teeth grade 2-3(Aminoshariae et al., 2020).
3. Severe periodontitis with potential for additional tooth loss in the superior maxilla and moderate periodontitis in the mandible(Caton et al., 2018) grade C and stadium 4.
4. Recession gingival Miller type 1 in all mandible teeth and mobility of teeth grade 1-2(Aminoshariae et al., 2020).
Differential fixed treatments
- Extract all teeth, wait one month for primary healing, and perform horizontal bone
regeneration with autologous bone and xenograft.
In the areas of 1.3, 1.4, 1.5, and 1.6, perform a block graft to seal the hole produced by the bullet.
Wait four months and place six implants.
- Extract all the teeth, wait a month for them to heal, and make a plate with the implants that will be fixed with micro-screws in the areas where there is bone, such as the maxillary flying abutments.
This is a good treatment, but it could have complications such as periodontitis(Nguyen, Caruhel and Khonsari, 2018).
Treatment
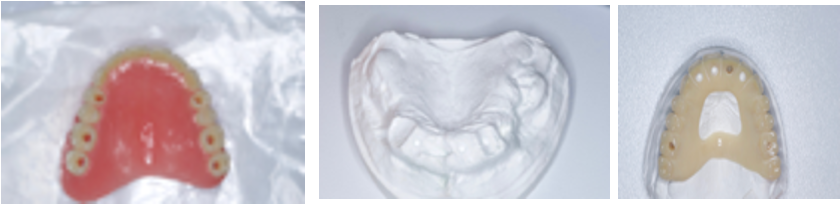
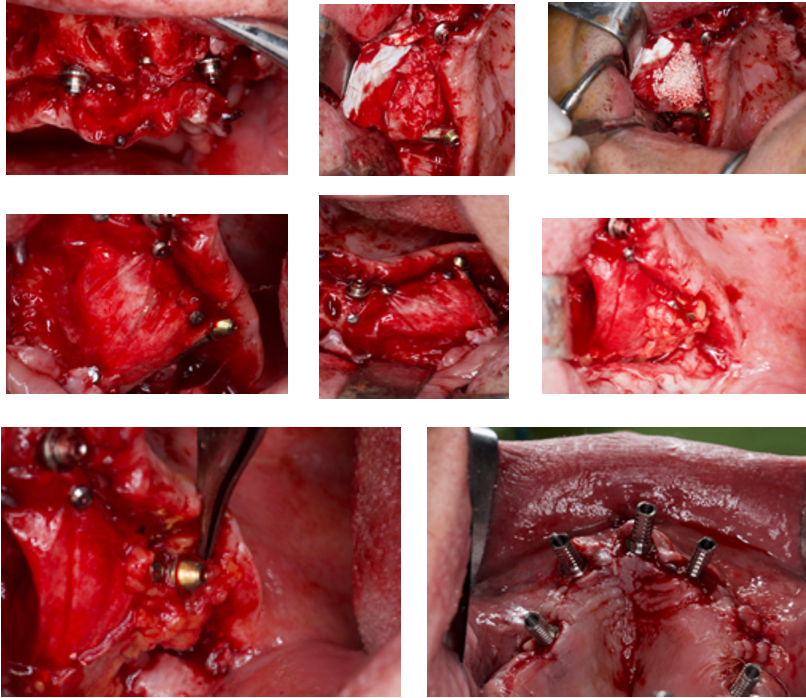
The Treatment carried out in the maxilla was:
1. Extract teeth, regularize bone, and place four active Nobel implants (Nobel Biocare, Kloten, Switzerland).
2. Perform a regeneration with autologous bone, filling the gaps between the implants and the buccal bone.
3. The respective multi-units were placed to correct the prosthesis’s emergence.
4. In the first quadrant, the defect in areas 1.3 to 1.6 was regenerated with autologous bone, xenograft and collagen membrane, fixed with thumbtacks.
5. In area 16, a zygomatic internal connection implant from Noris Medical (Noris Medical, Fuengirola, Spain) was placed with a 45º angled multi-unit.
It was covered around the zygomatic implant with the bichat ball to avoid a future recession of the tissues.
6. Once sutured, the temporary coping was placed on the multi-unit, and immediate loading was performed.
7. After two weeks, an all-on-four was performed on the jaw with the fast and excellent Nobel BioCare implants (Nobel BioCare, Kloten, Switzerland).
8. The patient used a night guard to prevent the break of their acrylic teeth even though
inserting dental implants in bruxers does not affect the implant failure rates(Chrcanovic, Albrektsson and Wennerberg, 2015).
9. After three years, performed “All On Four” Treatment in the mandible due to teeth loss for periodontal reasons.
Options
Conveniences
1. It is an effective treatment that works overtime(Yates et al., 2014)
http://What are all on 5 implants?.
2. Long implants, such as zygoma implants, are ideal implants to support immediate loading. (Paper and Implants, 2010)
3. The Bichat fad pad is used to avoid future recessions on zygoma implants(Guennal and Guiol, 2018).
4. The immediate loading increases the patient’s satisfaction with the Treatment (Mozzati et al., 2015; Abdunabi et al., 2019).
Inconveniences
1. Requires more manual skill. If there is a complication in the surgery with the eyes or the infraorbital nerve, the Treatment could have many consequences on the patient’s health(Candel-Martí et al., 2012).
2. It was performed under local anaesthesia, and achieving the lower and upper parts simultaneously was impossible. The ideal would have been to increase satisfaction and have the patient go through a single surgery.
3. The anaesthetist did not perform intravenous sedation due to the patient’s past with drugs; since he ran the risk of not producing an adequate soothing effect, the anaesthesia receptors were highly saturated by the drugs.
For this reason, it was performed under local anaesthesia and oral sedation.
Surgery/ Treatment details:
1. Anaesthesia local: Adrenaline 4%, infiltrative in the buccal zone, in the palatal gingivae was put anaesthesia in the main palatal nerve, Nasopalatal nerve and infraorbital nerve.
This case was realized under general anaesthesia.
2. Flap design:
Crestal incision with a buccal discharged on the 1.7.
3.Maxilla extractions.
4. Implants:
Upper Maxilla: Noris medical Zygoma implants, Nobel active implants.
Mandible: Nobel Biocare Speedy groovy implants.
5. The placement of the zygoma implants was realized in an internal sinusal position. However, In the crestal zone, the implants were not surrounded by bone, which classified the implant as ZAGA 4(Aparicio, 2011).
6. The Bichat fad pad surrounds the zygoma implant in the buccal position.
7. suture vicryl 4.0.
8. Immediate loading.
Oral medication:
1. The patient was premedicated with a dose of 500 mg with clavulanic acid 125 mg was the antibiotic of choice. It was administered every 8 hours for ten days, starting two days before.
2. Zamene 10 mg and Nolotil 575 mg were prescribed to control swelling and pain thirty minutes before the surgery.
3. A supplement of multivitamins for one month was prescribed.
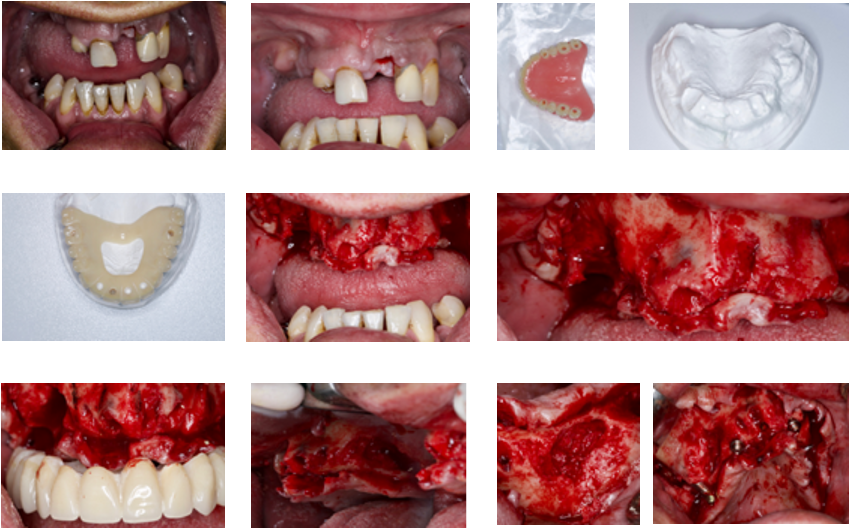
Steps to make the immediate prosthesis
1. Being such a complicated case, it was obtained by having two types of provisionals, one with complete teeth and palatal support and the other, a total prosthesis with pink gum—both with holes where the dental implants would be placed.
2. To perform both prostheses, the patient’s posterior teeth were removed; in this case, he had root remains.
3. A base plate plus impellers was requested.
4. Occlusion, vertical dimension, smile, midline, and canine lines were verified.
5. Once the above was verified, a teeth test was requested. This test only included the posterior teeth, but it would serve as a reference to perform the prosthesis.
6. Once all of the above was verified, the two prostheses mentioned above were requested.
7. I feared the prosthesis with the teeth on top would break, as it had a bilateral hole; if I broke the acrylic too much, the prosthesis would split. So, that is why I had the acrylic prosthesis complete.
Prosthesis photos
Photos of surgery:
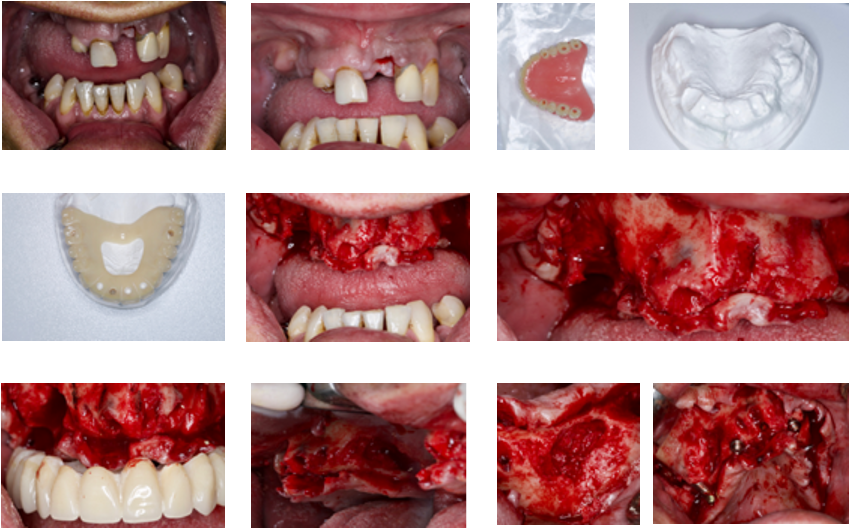
Definitive temporal prosthesis
Ultimately, the prosthesis used was that of complete teeth without pink gums. We were looking for this prosthesis to make it similar to natural teeth and weigh little, not overload the dental implants, especially the zygomatic.
Steps to adjust temporary fixed prosthesis screwed to the implants through the provisional loading cylinders.
1. Adjust the multiunits to the torque that the manufacturer recommends. In this case, Noris medical® zygoma has 25 Ncms and for Nobel active® implants 15Ncm for the angled ones.
2. A rubber dam protects the gum around the cylinders. Then, a white thermo-polymerizable acrylic is used, such as the Bredent® or tab 2000.
3. The prosthesis is attached to the cylinders, and we verified that none moved. Then, it can be sent to the laboratory to make the final prosthesis in high-impact acrylic polish.
Suppose we have used the acrylic of high impact on the capture of the cylinders if we verify that the vertical dimension, occlusion, and smile line are correct. In that case, we can mask the prosthesis, put it in the pressure cooker, and later polish the acrylic remains.
4. Once the prosthesis is finished, it is placed on the multiunits, torqued to 15 Ncm, Teflon is placed, and is covered with ultra-short composite.
5. Improving the colour and strength of the temporary prosthesis, apart from applying the Tab 2000 around the cylinders, was used throughout the occlusal area, making the teeth solid.
In the vestibular part, composite and adhesive were applied, and it was used in the cervical at 3.5 to make the teeth more accurate since the man did not want an A.3 colour as he had initially been saying.
Once the prosthesis is finished, it is covered with acrylic at the union of the cylinders with the gum. The idea is to leave a flat prosthesis where no concavities could accumulate food.

A photo of the temporal prosthesis after changing the colour with composite and Tab 2000® was needed to rebase the gaps between the platform of the implants and the prosthesis.
Photo of metal-ceramic mandible all on four treatments

Final prosthesis at four years check-up: The patient wears an all-on-four on conventional implants.
Periodontal re-evaluation:
1. The aims for this Treatment were not completed:
A. The aim is to reduce Bleeding and plaque levels to £25%. The patient never used an electric brush, and he returned after the first year of treatment once when all lower teeth had mobility grade 3.
B. The deep pocket was not more significant than 5mm in the maxilla but more than that in the mandible.
C. There was pain and a foul smell from the mandible; the upper rehabilitation was stable.
2. The patient has not stopped smoking; however, the upper rehabilitation was stable, not peri-implantitis or mucositis.
3. The lower rehabilitation was performed due to his periodontal disease; after the first year, the patient did not come back to consultation until he had pain in the mandible.
4. the patient must be re-educated in oral hygiene and stop using cigarettes. The patient will be scheduled in six months for periodontal maintenance if necessary.
Evolution and prognosis:
In this case, the prognosis is reserved. It depends a lot on the patient. The prostheses were tried to make the least retentive possible so the patient could use the water pick and the brush without problems.
The patient was given an appointment every six months. However, he attended a consultation once a year after performing the prosthesis below.
Overall:
In this case, he learned, above all, to manage the patient’s medical regimen since the effect of the anaesthesia lasted very little. At the end of the hour, he had to medicate with a dipyrone to relieve the pain. The maximum number of cárpule placed was 10.
The patient did not have significant postoperative discomfort and had not lost any implants four years after the zygoma surgery.



