All-on-six, nasal fossa lift, bone regeneration, implants, definitive prosthesis, nasal lift technique for augmentation

Referral
A general dentist from a dental clinic in Alcoy (Alicante, Spain).
Patient Complaint
“I want fixed teeth and not wear the removable prosthesis; I have a bad smell of the mandible.”
History of presenting complaints
1. The patient lost his upper teeth 20 years ago.
2. He underwent dental implants ten years ago, but the Treatment failed after three years.
The patient visited different specialists, but they told him that He did not have enough bone to put dental implants.
3. The patient knows he has a problem. He did not feel good about his lower implants.
He gets pus, food often makes him sick, and lately, he has stomach problems.
Social and medical history
Age: 53 years old.
Married: 23 years old.
Occupation: Rigger.
Actual diseases: Diabetes type 2.
Past illnesses: None.
Allergy: Pollen.
Familiar condition: Diabetes type 2(Aghaloo et al., 2019); his mother lost a leg due to diabetes.
Smoke: He smokes ten cigarettes per day.
Dental history
Oral hygiene technique: Inadequate.
Dental visits: One every year in the last years.
Reasons for loss of teeth: Periodontal disease.
Oral pain: In the mandible.
Habits: Not refer.
Evaluation:
1. Health
2. Function
3. Aesthetics
Dental treatments performed before surgery
- Periapical radiographs.
2. Orthopantomography.
3. Perio-Chart:
A. The patient has a pocket depth of over 6 mm in 4.1, 3.1 and 3.2 implants.
B. Implant 4.1 has grade 2-3 mobility.
C. It presents bleeding or plaque in the first inspection; it bleeds when performing a periodontal probing.
D. CPITN code was from the mandibular anterior teeth 4.
I. Radiographic interdental bone loss: There is an extension of bone loss to the middle third of the implant, and it is almost apical in 3.1 and 4.1.
J. Loss of teeth: Teeth were lost due to periodontal reasons.
K. CAL values were ³5 mm.
4. Scaling and root planning were performed; the aims for this treatment are:
A. To reduce bleeding and the level of plaque to £25%.
B. To reduce the depth level of the pocket under 5 mm.
C. To prevent pain or bad smell.
E. To evaluate other techniques, such as regenerative surgery and implant extraction.
5. The patient was taught about motivation and education about the harmful effects of tobacco and alcohol on her health. It was recommended to visit pages such as the Slutta.no page, created by Helsenorge.no, for more information about stopping smoking. Pinto-Filho et al. 2018(Pinto-Filho et al., 2018) conducted a cross-sectional study about alcohol and tooth loss; they found that Alcohol dependence increased 2.5 times the risk of tooth loss.
6. Sistematic revaluation will be done after four months to check the periodontal conditions.
7. Diabetes increases the pathology of the perimplantitis(Schwarz et al., 2018).
Attitudes Towards Previous Treatment
Cooperative attitude.
Features
1. Skin colour and complexion Gypsy man features.
2. Brachyfacial features.
3. The patient presents click(De Rossi et al., 2014) in the oral opening without displacement or pain.
Mouth:
1. strong chewing muscles present pain on palpation and are related to his bruxism(Lavigne et al., 2008).
2. Normal saliva, tongue, and the floor of the mouth is hydrated.
3. Sun dehydrated lips.
O.P.G before surgery:

O.P.G after removing dental implants infected:

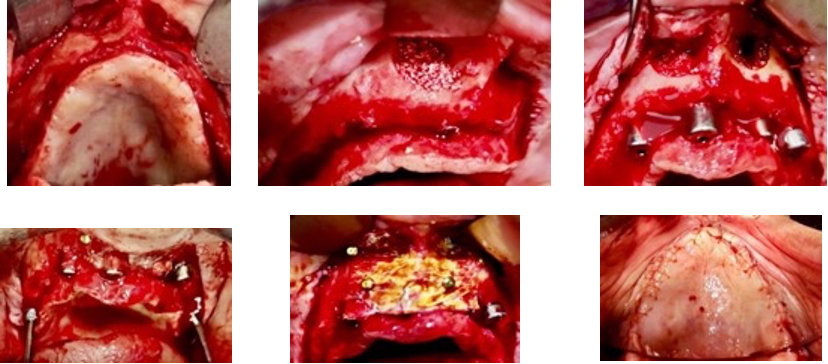
Photos of the surgery:
Diagnosis
1. Atrophic in the anterior maxillary zone(Prato et al., 2004).
2. Active periimplantitis(Caton et al., 2018) localised in the mandible with the influence of diabetes, stadium 4 grade C.
3. Bruxism.
Differential fixed treatments
- Quad zygoma rehabilitation.
- Two anterior zygomas and two pterygoids.
- Four Straumann implants of 4mm, regeneration with Bio-Oss and collage membrane plus Pins in the anterior maxilla. Two pterygoid implants with a multiunit of 30º. They were discarded because the patient had that kind of Treatment with small implants and failed.
- Regeneration with Gore-Tex or metal membrane, wait nine months and put six short implants(Ravidà et al., 2019). Discarded, it is too expensive, and it is complicated to get regeneration in the palatal bone zone (Khoury and Hanser, 2019).
- After removing all implants from the mandibular jaw, bone regeneration would be done; after four months of regeneration, “All on four” rehabilitation with acrylic material will be realised.
The patient ruled it out because he did not want to wear a complete denture for eight months until the dentist fixed his lower teeth.
Treatment
1. Nasal fossa elevation, placement of two long Klockner implants.
2. Regeneration with autologous bone and regeneration with bio-oss and Perioguide membrane. (Nicoli et al., 2019)The membrane was moistened with iodoform, and the surgeon soaked the bone with vancomycin.
3. In the posterior zone, two implants were set in 1.5 and 2.5 with multiunit 30º.
4. removing the implants with mobility, cleaning everything, and autologous bone was settled in the bone defects.
5. After seven months, it was settled that a new implant in the mandible and a removal overdenture(Di Francesco et al., 2019) supported by three implants were designed.
6. The patient was informed of needing an MRI of his temporomandibular joint. In addition, he was referred to a physiotherapist for facial and joint massage.
7. Using a myorelaxant discharge splint et al. et al.(Jokubauskas, Baltrušaitytė and Pileičikienė, 2018) when he was relaxed watching TV or doing work on the computer, and he did not need to speak and had the prostheses in place.
Options
Conveniences
1. Long implants in vomer or eminence canine permit good stability.
2. “All on-six” rehabilitation can be supported with two long nasal implants and a fixed prosthesis (Nicoli et al., 2019).
3. In four months, the prosthesis can be made from 1.5 to 2.5 or 2.6 to 1.6 with a cantilever less than one mm(Jensen et al., 2015).
Inconveniences
1. It Requires more manual skill, and the elevation of the nostrils is painful and requires taking bone from the ramus, with the consequent risk of altering the lingual or inferior dental nerve (Davó et al., 2018).
2. It is necessary to know the prosthodontics because otherwise, the appearance of the implants can make it challenging to perform the prosthesis and affect its sanitation, causing peri-implantitis (Schwarz et al., 2018).
Surgery/ Treatment steps:
1. Anaesthesia
A. Ramous graft: Block inferior dental nerve with lidocaine 2%, infiltrative buccal, lingual zone.
B. Nostril: block infraorbital nerve, infiltrative buccal and palatal, greater palatine and nasopalatine nerves.
2. Flap design
Buccal frenulum incision and crestal incision until 2.7 and 1.7.
3.Suture
4.0 resorbable
4.Implants
essential cone 1.5 (Klockner, Barcelona, Spain).
Postoperative instructions
1. Amoxicillin 1 gram every 12 hours for six days.
2. Zamene 30 mg 1 every 12 hours for one day.
3. Nolotil 500 mg 1 every eight hours for three days.
4. Soft diet for ten days.
5. Put ice on his face for 3 hours on the first day and 2 hours on the second day, with intervals of 5 minutes.
6. supplement of vitamin D(Machado et al., 2020) for helping with periimplantitis and bone regeneration.
Ct scan post six months of treatment:
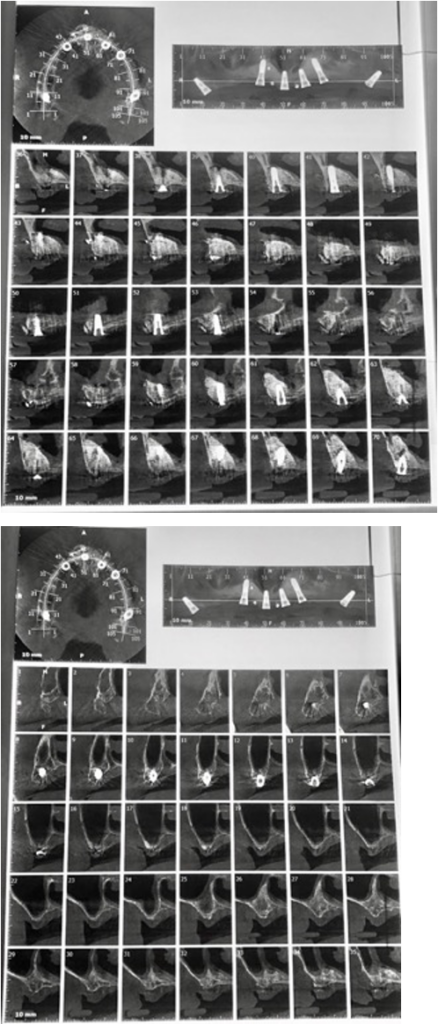
O.P.G after eight months of surgery:

Periodontal re-evaluation after six months:
1. The aims for this treatment were completed:
A. To reduce bleeding and the level of plaque to £25%.
B. To decrease the depth level of the pocket to less than 4mm.
C. To eliminate pain or bad smell.
D. As seen in orthopantomography, the incisal implant extraction and the subsequent regeneration allowed another implant to be placed at 31. This treatment will lead to an overdenture on a supported bar in 3 implants.
Unfortunately, these implants could not be saved because the bone losses were profound, and there was much infection in the area.
2. the patient needs to be re-educated in oral hygiene. The patient will be scheduled in six months for periodontal maintenance if necessary.
Evolution and prognosis
The prognosis is good because all implants had good stability and clinical aspects after six months.
The definitive prosthesis must be given to the patient in November 2021, after almost one year of implant placement, because the patient travels and has few visits to the dentist.
The patient must come once a year to clean the prosthesis and change the screws if needed.
The patient came. I said he did not have money for a new prosthesis in metal-porcelain, so I adapted a complete prosthesis with a cylinder to unite the prosthesis with the multiunits.
Photos of a complete prosthesis readapted to the implants.

Adjust the temporary complete prosthesis to a fixed prosthesis screwed to the implants through the provisional loading cylinders.
1. Adjust the multiunits to the torque that the manufacturer recommends. In this case, in Klockner, it is 35 Ncm for the straight multiunits and between 15-20 Ncm for the angled ones.
2. The second step involves placing the healing cups on the multiunit ones. The Klockner ones are too high, but the latter are used since they are compatible with the Nobel Biocare ones.
3. We apply heavy silicone on the prosthesis, which we have previously verified that its occlusion does not vary with the placement of the multiunit. If it does, the prosthesis must be retouched to make room for the multiunit.
We want to see where the multiunit would come out in the prosthesis.
4. The multiunit position has been marked on the silicone. We make some holes in it, which will be the spaces occupied by the metal cylinders that are screwed onto the multiunits.
5. A rubber dam protects the gum around the cylinders. Then, a pink thermo-polymerizable acrylic, such as the Bredent® or the Respal NF®, is used to join said cylinders to The prosthesis. If these acrylics for prostheses are not available, they could be joined with structure II or tab 2000.
6. the prosthesis is attached to the cylinders, and we verify that none of them move. Then, it can be sent to the laboratory to make the final prosthesis in high-impact acrylic polish.
Suppose we have used the acrylic of high impact on the capture of the cylinders if we verify that the vertical dimension is correct, occlusion, and smile line. In that case, we can mask the prosthesis, put it in the pressure cooker, and later polish the acrylic remains.
7. Once the prosthesis is finished, it is placed on the multiunits, torqued to 15 Ncm, Teflon is placed, and is covered with ultra-short composite.
Overall:
In this case, I learned that angulation of the implants achieves better primary stability in cases where there is not much bone left.
Using angled multi-units allows for correcting angulations that could not otherwise be rehabilitated.
I learned that diabetes, although controlled, is a disease that interferes with the healing of the bone and gum; generally, at six months, the prosthesis should have been done, but in this case, it was decided to wait longer because it was not clear what the bone was perfect, therefore, and due to implants would fail, the measurements were delayed for two more months.
Final photo




