Introduction
At Facialia.com, we specialize in advanced periodontal treatments that restore both function and aesthetics. This clinical case highlights a comprehensive approach to treating gum recession using the connective tissue graft, Emdogain, and the tunnel technique, from diagnosis through post-operative maintenance.
Patient’s Main Complaint
A 46-year-old patient visited our clinic in Valencia, Spain, presenting with:
- Generalized tooth mobility
- Bleeding gums and pus discharge
- Bad breath
- Increasing dental sensitivity, especially in teeth 2.1 and 2.2
- Gum recession
Medical and Social History
- Medical Background: Bruxism, depression, past COVID-19, psychosis
- Habits: Nail biting, daily snus use (previously smoked 20 cigarettes/day)
- Alcohol Use: Increased during depressive episodes
- Allergies: Pollen
- Occupation: Unemployed
Initial Clinical Assessment
Clinical and radiographic evaluations showed:
- Miller Class I–IV gum recessions
- Thin periodontal biotype
- Pocket depth and bone loss >15%
- Mobility grade 2 in multiple teeth
- High plaque and bleeding indices
Phase 1: Supragingival Control and Patient Education
This stage focused on biofilm removal and motivation for behavioral change:
- Professional cleaning and airflow
- Instruction in effective brushing techniques (electric toothbrush recommended)
- Disclosing tablets to track plaque removal
- Scaling and root planing
- Education on the risks of smoking and alcohol consumption
Diagnosis
Based on Miller’s classification:
- Class I: Teeth 4.4, 4.5, 4.2, 1.3, 2.3, 1.4, 1.5
- Class II: 3.4, 3.5
- Class III: 1.1, 1.2, 2.2, 2.4, 2.6
- Class IV: 4.1
Also diagnosed with bruxism and a reduced periodontium.
Phase 2: Subgingival Instrumentation
Scaling and root planing were performed with chlorhexidine irrigation. The goal was to:
- Reduce probing depth to <4 mm
- Decrease plaque and bleeding levels to ≤25%
Phase 3: Connective Tissue Graft Surgery
We proceeded with a connective tissue graft using the tunnel technique combined with Emdogain to enhance healing and soft tissue regeneration for the gum recession:
- Local anesthesia and cleaning
- Tunneling flap created from 2.1 to 2.6
- Subepithelial graft harvested from palatal area (1.3 to 1.5)
- Emdogain applied to recipient site
- Graft stabilized with suspensory sutures
Postoperative Care and Medications
- Paracetamol 500 mg three times daily (3 days)
- Vitamin D supplement to support bone healing
- Hyaluronic acid oral rinses to aid gingival repair
Prognosis and Reevaluation
Results included:
- Reduced dental sensitivity in 2.1, 2.2, and 2.3
- Increased keratinized gingiva
- Composite veneer placed in 2.4 for aesthetics
However, the patient continued alcohol and snus use, requiring motivational reinforcement in the next phase.
Follow-up and Complications
Two years later, the patient returned after unsuccessful regenerative surgery in London, with persistent inflammation around tooth 1.2. We decided to wait for tissue maturation before any further surgical intervention.
Maintenance Phase
Maintaining periodontal stability is essential. The patient is now under a structured follow-up program with:
- Regular hygiene checks
- Periodontal charting and radiographs
- Treatment adaptation if relapse occurs
Conclusion
This case illustrates how gum recession can be successfully treated using a connective tissue graft, Emdogain, and the tunnel technique. The success of this method depends not only on the surgical approach but also on patient cooperation, motivation, and long-term maintenance.
Why Choose Facialia.com for Gum Recession Treatment?
At Facialia.com, we offer expert solutions for gum recession, using evidence-based approaches like connective tissue grafting and Emdogain therapy. Whether you suffer from sensitivity, aesthetic concerns, or advanced recession, our tailored treatments can help you restore your smile and comfort.
Book your consultation today at Facialia.com and take the first step toward lasting periodontal health.

Initial OPG

Photo second quadrant

Periapical Antero- Inferior teeth

Surgery photos

Plaque index

Second quadrant


Periapical X-rays
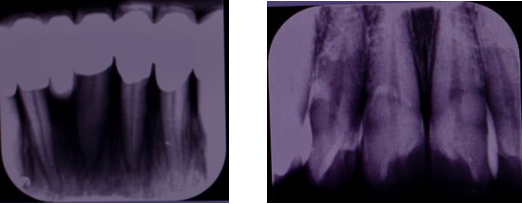
The lesion in 1.2





