Clinical Case Report: Comprehensive Management in Periodontal Disease and Peri‑implantitis
Abstract
This report presents a scientifically based, multidisciplinary approach to managing a 46‑year‑old male patient with advanced periodontal disease and peri‑implantitis. Utilizing evidence‑based techniques such as the Khoury technique, Kasanjian vestibuloplasty, guided bone regeneration, and the use of collagen membranes with dental implants, our treatment protocol is at the forefront of modern dental science. Facialia Clinic – Advanced Periodontal and Implant Treatments in Silla, Valencia leads the way in delivering innovative care.
Introduction
Managing complex periodontal conditions and peri‑implantitis demands a structured and research‑driven treatment plan. In this case, after previous implant failure and recurrent peri‑implantitis, a comprehensive, phased approach was implemented. This protocol emphasises strict biofilm control, precise surgical interventions, and regenerative procedures that are supported by numerous scientific studies. At Facialia Clinic – Advanced Periodontal and Implant Treatments in Silla, Valencia, we combine cutting‑edge research with clinical expertise to ensure long‑term stability and improved aesthetics. Our commitment to excellence is evident in every step of our process at Facialia Clinic – Advanced Periodontal and Implant Treatments in Silla, Valencia.
Patient History
Chief Complaint:
The patient stated,
“I do not want to use the removable prosthesis. I had dental implants that failed two years ago, and now no one will place new implants because they say I do not have enough bone.”
At Facialia Clinic – Advanced Periodontal and Implant Treatments in Silla, Valencia, we understand the profound impact that implant failure can have on quality of life.
Presenting History:
- The patient previously underwent implant treatment with bone regeneration.
- A recent implant loss rendered his prosthesis unusable.
- The initial diagnosis of peri‑implantitis led to a recommendation for a removable appliance.
Personal Information:
- Age: 46 years
- Gender: Male
- Marital Status: Single
- Occupation: Electrical Engineer
Medical & Social History:
- Medical Conditions: Psoriasis; history of severe respiratory infections.
- Allergy: Clavulanic acid
- Family History: Includes senile dementia, myocardial infarction, and depression.
- Lifestyle: Social alcohol consumption (one glass of wine daily) and smoking (15 cigarettes per day); obstructive sleep apnoea.
At Facialia Clinic – Advanced Periodontal and Implant Treatments in Silla, Valencia, a thorough review of the patient’s history is crucial for tailoring an individualised treatment plan.
Clinical and Radiographic Examination
Extraoral and Intraoral Findings:
- The patient exhibits brachy‑facial features with strong masticatory muscles.
- Salivary flow, tongue mobility, and mucosal hydration are within normal limits.
Radiographic Findings:
- Detailed imaging (periapical, panoramic, and CBCT) revealed significant bone loss around implant 3.2 (exceeding 80%) and deep periodontal pockets in multiple regions.
- Gingival recessions and endodontic‑periodontal lesions, notably on tooth 4.3, were also observed.
These findings reaffirm our evidence‑based approach at Facialia Clinic – Advanced Periodontal and Implant Treatments in Silla, Valencia.
Diagnosis
- Implant 3.2: Advanced peri‑implantitis with severe bone loss.
- Periodontal Disease: Severe periodontitis with a molar‑incisor distribution pattern.
- Endodontic‑Periodontal Lesion: Tooth 4.3 with grade 3 mobility and apical involvement.
- Alveolar Atrophy: Notable anterior mandibular bone loss with a deficiency of keratinised gingiva.
At Facialia Clinic – Advanced Periodontal and Implant Treatments in Silla, Valencia, our diagnostic process is rooted in current scientific literature.
Treatment Plan and Phases
Phase I: Initial Therapy and Biofilm Control
Key objectives were to:
- Educate the patient on optimal oral hygiene (brushing, flossing, and plaque detection techniques).
- Eliminate supragingival biofilm and address modifiable risk factors such as smoking and alcohol intake.
- Conduct a six‑week reevaluation to monitor behavioural changes and plaque control.
This meticulous phase sets the foundation for success at Facialia Clinic – Advanced Periodontal and Implant Treatments in Silla, Valencia.
Phase II: Periodontal Intervention
Focused on subgingival instrumentation through scaling and root planing, this phase aimed to:
- Reduce periodontal pocket depths and control bleeding on probing.
- Enhance plaque removal with adjunctive chemical and physical agents.
- Reassess periodontal status after one month for further decision‑making.
The precision of our interventions is a hallmark of Facialia Clinic – Advanced Periodontal and Implant Treatments in Silla, Valencia.
Phase III: Surgical Interventions and Regeneration
Owing to persistent peri‑implantitis and periodontal challenges, the following procedures were executed:
- Extraction of tooth 4.3 and implant 3.2 due to extensive bone loss.
- Resective periodontal surgery employing a flap technique to remove granulation tissue and reshape the alveolar bone.
- Bone regeneration using autologous bone grafts combined with xenograft material.
These advanced surgical protocols exemplify the state‑of‑the‑art treatments available at Facialia Clinic – Advanced Periodontal and Implant Treatments in Silla, Valencia.
Advanced Surgical Techniques
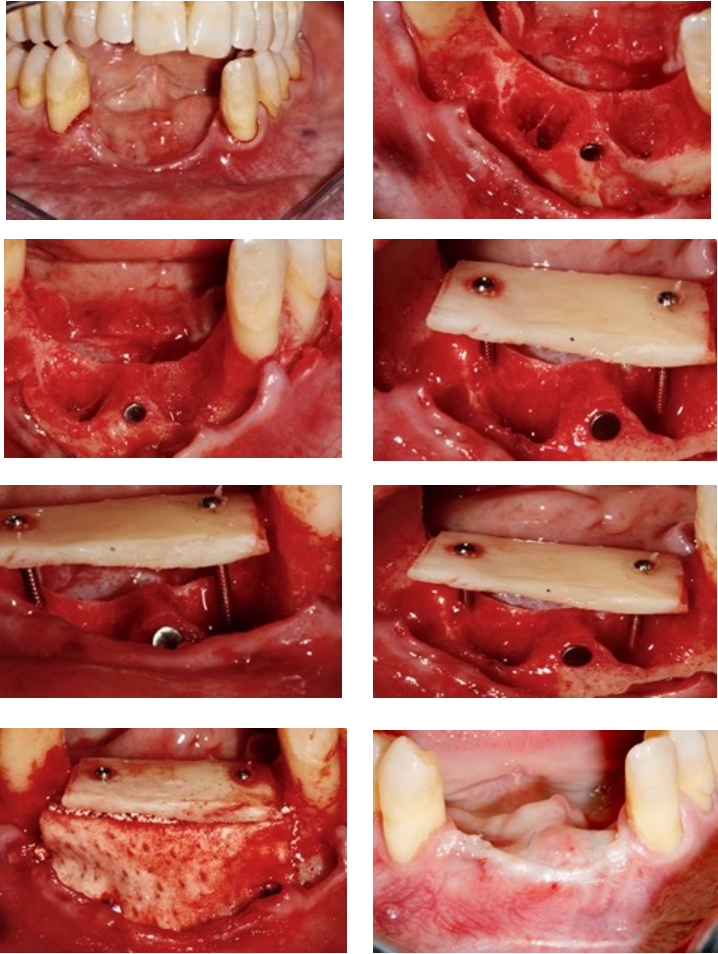
Khoury Technique
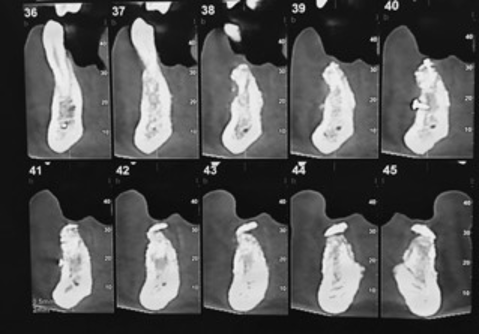
Vertical bone augmentation was achieved using the Khoury technique, which utilises autogenous bone grafts stabilised with micro‑screws to facilitate vertical regeneration. This method is supported by robust scientific research and is a core service at Facialia Clinic – Advanced Periodontal and Implant Treatments in Silla, Valencia.
Periodontal Disease Management
Our comprehensive strategy for managing periodontal disease involves meticulous plaque control, behavioural modifications, and regular maintenance visits—all critical to preventing further deterioration. Trust Facialia Clinic – Advanced Periodontal and Implant Treatments in Silla, Valencia for evidence‑based care.
Peri‑implantitis Treatment
Combining non‑surgical debridement with surgical interventions, our approach aims to eradicate biofilm, reduce inflammation, and promote re‑osseointegration around the implant site. This balanced strategy is a key feature at Facialia Clinic – Advanced Periodontal and Implant Treatments in Silla, Valencia.
Kasanjian Vestibuloplasty
Kasanjian vestibuloplasty was performed to deepen the vestibule and expand the zone of keratinised gingiva, improving both function and aesthetics. This technique, which involves the removal of excess muscle fibres and placement of a connective tissue graft, is a distinctive procedure at Facialia Clinic – Advanced Periodontal and Implant Treatments in Silla, Valencia.
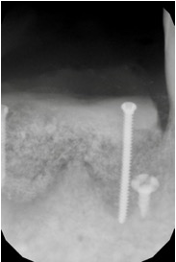
Dental Implants
Following successful bone regeneration and periodontal stabilisation, new dental implants were precisely positioned to restore function and aesthetics. Our implant protocols reflect the latest scientific advances and are executed at Facialia Clinic – Advanced Periodontal and Implant Treatments in Silla, Valencia.
Guided Bone Regeneration
Guided bone regeneration (GBR) is integral to our regenerative protocol. By combining autologous bone, xenograft material, and barrier membranes, we create the ideal conditions for bone healing. This sophisticated technique is a specialty of Facialia Clinic – Advanced Periodontal and Implant Treatments in Silla, Valencia.
Collagen Membrane
A collagen membrane was used to protect the grafted area from soft tissue invasion, ensuring optimal space maintenance for bone regeneration. This advanced material is a key component of the procedures performed at Facialia Clinic – Advanced Periodontal and Implant Treatments in Silla, Valencia.
Facialia Clinic – Your Trusted Centre in Silla, Valencia
At Facialia Clinic – Advanced Periodontal and Implant Treatments in Silla, Valencia, we specialise in the comprehensive management of periodontal disease and peri‑implantitis. Our state‑of‑the‑art facility, located at Avenida Reyes Catolciso, 3, Silla, Valencia, offers cutting‑edge treatments that are firmly grounded in scientific research.
- Telephone: 961776426
- Website: facialia.com
Choose Facialia Clinic – Advanced Periodontal and Implant Treatments in Silla, Valencia for personalised, high‑quality dental care that delivers exceptional functional and aesthetic outcomes.
Outcome and Follow‑up
The patient was enrolled in a supportive periodontal care programme with regular reviews every three to six months. Outcomes included:
- Stabilisation of periodontal pockets and significant improvement in oral hygiene.
- Successful bone regeneration and an increase in keratinised tissue around the newly placed implants.
- A commitment to ongoing lifestyle modifications, such as reduced smoking and improved oral care routines, ensuring long‑term success with Facialia Clinic – Advanced Periodontal and Implant Treatments in Silla, Valencia.
Periapical tooth 4.3

CBCT
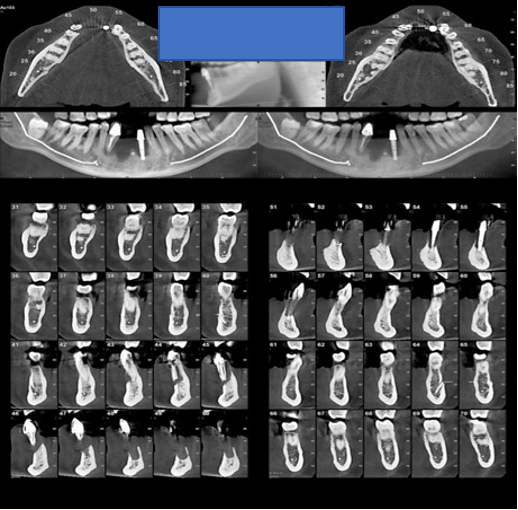
Periapical series
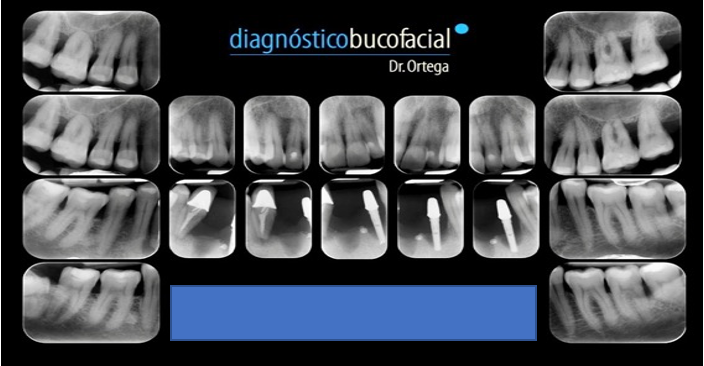
Phase two
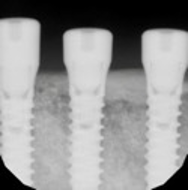
O.P.G. control of regeneration

C.B.C.T. scan after three months
X-ray after three months
Photos of the surgery
Periapical X-ray with the implants
Photos of implant surgery
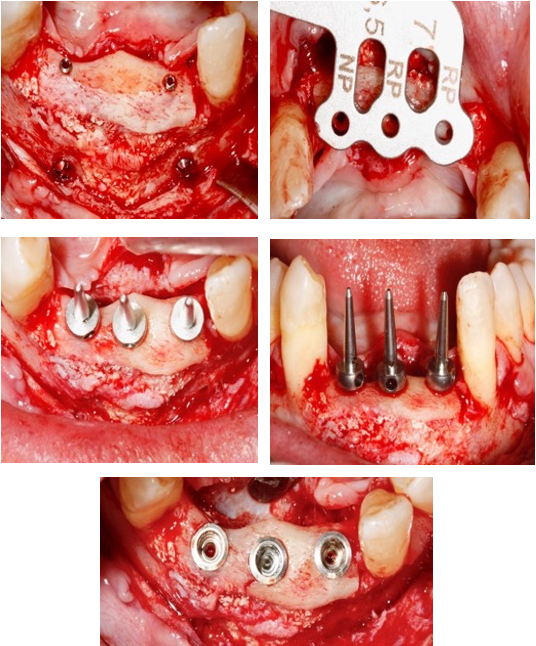
It waited four months to place the dental implants. The second phase was done three months later. A vestibuloplasty with a connective tissue graft was performed to obtain buccal sulcus and keratinised tissue with the aesthetic result.
O.P.G. with the implants

Photos with the implants after Kazanjian Vestibuloplasty

Photo baseline vs post-treatment

Conclusions
This case underscores that a structured, phased approach—backed by scientific evidence—can effectively manage complex periodontal conditions and peri‑implantitis. Advanced techniques, including the Khoury technique, Kasanjian vestibuloplasty, guided bone regeneration, and the use of a collagen membrane in conjunction with dental implants, are essential for achieving long‑term stability and superior aesthetics. The patient’s active participation and adherence to our maintenance programme were key to treatment success. For exceptional periodontal and implant care in Silla, Valencia, trust Facialia Clinic – Advanced Periodontal and Implant Treatments in Silla, Valencia. Contact us today on 961776426 or visit facialia.com to learn more about our innovative dental solutions.



