Authors: Alejandro Rey Dintrans Nº Colegiado 28009651

and Mauricio Sanchez Nº Colegiado 28008532

Referral
The patient attends a private clinic in (Madrid, Spain).
Patient Complaint
«I do not want to use the removable prosthesis. »
History of presenting complaints
The patient has no upper teeth in the first quadrant. The patient used a removable prosthesis and did not want to use it.
Social history
Age:45 years old.
Marriage: 20 years.
Occupation: Executive manager.
Medical history
Actual diseases: None.
Past illnesses: Nothing relevant.
Allergy: Horses hair.
Family conditions: Hypertension.
Alcohol intake: Social drinker, seven beers per week.
Tobacco: He smoked 30 cigarettes per day.
Dental history
Oral hygiene technique: Adequate
Dental visits: Frequent
Reason for loss of teeth: Chronicle periodontitis.
Habits: He wants to eat “pipas” (seeds of girasol).
Evaluation:
1. Health
2. Function
3. Aesthetics
The maximum aperture was 38 mm in the anterior zone.
Dental treatments performed before surgery
- Periapical radiographs.
2. Orthopantomography and CBCT.
3. Perio-Chart:
A. The patient had deep pockets of 5 mm on average in the maxilla; in the mandible were 4 mm.
B. The patient had a bridge from 2.1 to 2.5; the mobility grade was impossible to test 2(Aminoshariae et al., 2020).
C. Presented bleeding and plaque generalized.
D. CPITN code was from the mandibular teeth 1; the maxilla was 2-3.
E. Radiographic interdental bone loss: There is an extension of bone loss of less than 15% in the coronal third of the teeth in the maxilla.
F. In the mandible, the periodontal disease is an initial periodontitis with CAL values less of 4mm.
J. Loss of teeth: The first quadrant was lost due to periodontal reasons.
K. CAL values were £5 mm in the maxilla.
L. Presence of a chronic apical cyst without levels 2.1 and 2.2 symptoms.
4. Scaling and root planning were performed; the aims for this treatment are:
A. To reduce bleeding and the level of plaque to £25%.
B. To reduce the depth level of the pocket to under 5 mm.
C. Keep the horizontal defect under 2-3 mm in the furcation.
D. To prevent pain or bad smell.
E. To evaluate other techniques, such as regenerative or resective surgery, if this treatment is unsuccessful in the periodontal revaluation carried out after four months.
5. The patient was taught motivation and education about the harmful effects of tobacco and alcohol on her health. It was recommended to visit pages such as the Slutta.no page, created by Helsenorge.no, for more information about stopping smoking. Pinto-Filho et al. 2018(Pinto-Filho et al., 2018) conducted a cross-sectional study about alcohol and tooth loss; Alcohol dependence increased 2.5 times for tooth loss.
7. Sistematic revaluation will be done after four months to check the periodontal conditions.
Dental treatments needed to be after surgery
Possible re-endodontic treatment of 2.2, extractions of rootless on 3.8 and 3.6.
Attitudes towards previous treatment
Good attitude
Systematic orofacial examination
The face:
Skin colour and complexion of a white man.
Brachyfacial
Mouth:
Without swelling or tenderness.
Sufficient saliva and good mobility of the tongue. You have not presented tissue lesions in the soft tissues due to dry mouth (Wang, Thomson and Craig, 2020).
CBCT scan before surgery:
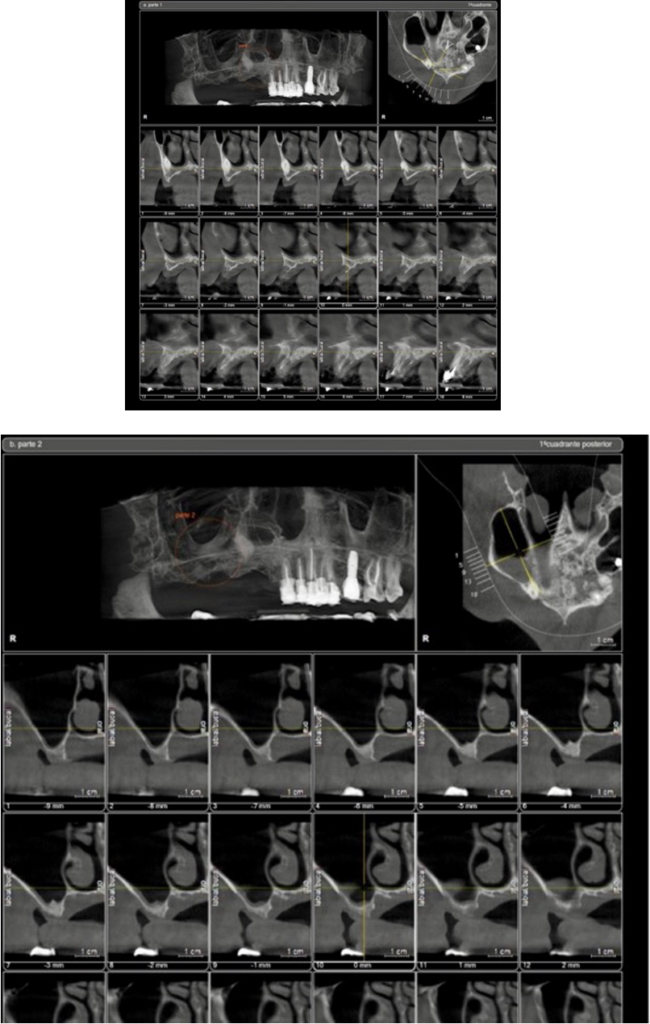
Diagnosis:
1. Atrophic bone in the maxilla includes canine and periapical chronicle abscesses in 2.2 and 2.1.
- Severe Periodontitis localized in the maxilla with potential teeth loss( Due to his first quadrant for periodontal pathology), stadium three and grade C(Caton et al., 2018).
Differential fixed treatments:
1. Elevation of the nostril, horizontal and vertical bone regeneration, placement of keratinized gingiva and conventional implants.
2. Sinus lift (Sáez-Alcaide et al., 2017)with autologous bones and xenograft, wait six months and place 3-4 conventional implants.
Treatment:
The treatment choice was to put two zygomas and to load with Galiimplant Zygoma internal connection immediately; however, the treatment which was done was:
1. The placement of Galiimplant Zygoma (Galiimplant, Lugo, Spain).
2. Perform a nasal membrane elevation and regenerate with autologous bone xenograft, mixed with phase one plasma rich in growth factors and put two BTI internal connection implants(Nicoli et al., 2019) (BTI Alava, Spain)
3. A fibrin membrane extracted from platelet-rich plasma was placed as the membrane to cover the regenerated area.
4. The zygomatic implant was covered with the Bichat fad pad(Guennal and Guiol, 2018) to avoid a possible recession in the future since the zygomatic implant was placed in ZAGA class 4.
Immediate loading was done with acrylic teeth. After eight months, a metal-porcelain bridge was performed.
Options (conveniences- inconveniences)
Conveniences
1. It is an effective treatment that works overtime(Yates et al., 2014).
2. Long implants, such as zygoma implants, are ideal implants to support immediate loading. (Paper and Implants, 2010)
3. The plasma rich in growth factors has been demonstrated to improve wound healing (Attia et al., 2020).
4. The Bichat fad pad is used to avoid future recessions on zygoma implants(Guennal and Guiol, 2018).
Inconveniences
1. Requires more manual skill. If there is a complication in the surgery with the eyes or with the infraorbital nerve, the treatment could have many consequences on the patient’s health(Candel-Martí et al., 2012).
2. general anaesthesia has risks, like pulmonary collapse and increased anxiety(Almeida, Salvoni and França, 2017; Eichelsbacher et al., 2018).
Surgery/ Treatment details:
1. Anaesthesia local: Adrenaline 4%, infiltrative in the buccal zone, in the palatal gingivae was put anaesthesia in the main palatal nerve, Nasopalatal nerve and infraorbital nerve.
2. This case was realized under general anaesthesia.
3. Flap design:
Crestal incision with a buccal discharged on the 1.7.
4.Suture 4.0 is resorbable.
5. Zygoma implant: Galiimplant Zygoma (Galimplant, Lugo, Spain)
The placement of the zygoma implants was realized in an external sinusal position.
Classified as ZAGA 4(Aparicio, 2011).
A Noris Medical Bur used it to design the way the zygoma through the external sinus.
Oral medication:
- The patient was premedicated with a dose of amoxicillin 750 mg, administered every 8 hours for 10 days, starting two days before the surgery.
2. Dexamethasone 4 mg twice a day for three days.
3. Nolotil 575 mg, three times a day for three days.
4. Rinses with a mouthwash with hyaluronic acid thrice a week and a Vitamin D supplement for bone healing and periodontal disease(Ghaly, Hart and Lawrance, 2019; Machado et al., 2020).
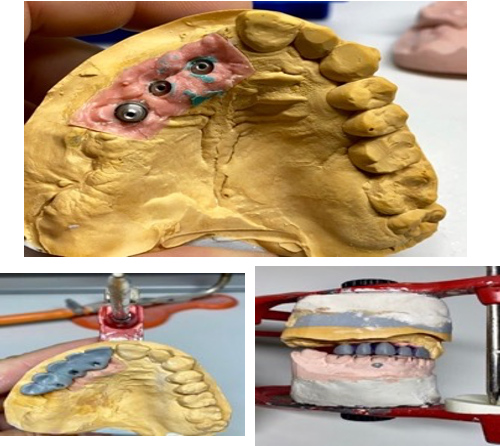
Steps to design the provisional prosthesis
Once the patient accepted the treatment and the budget, the first step was to take an alginate impression since the teeth were fragile and the entire upper bridge could come off. With this impression, we asked the laboratory to design a removable acrylic appliance for me. With holes in the palatine and support in the palate, without pink gums, for immediate loading of the first quadrant.
The palatal support should be highlighted since the device would move too much without this support, and it would not be easy to position it correctly.
In this case, no test for rims or teeth in pink gums was requested because there was no way to prove it. The patient did not want to be without teeth at any time, so his teeth were duplicated. The palatal support was added to position it and drill it in the middle to allow space to place the cylinders and later, the acrylic tap 2000.
Photo of provisional prosthesis

The pencil allows us to mark the ideal position for the emergence of the implants; this is extremely important to prevent the implants from invading an interproximal space in the final prosthesis, compromising aesthetics.
Photos of surgery:
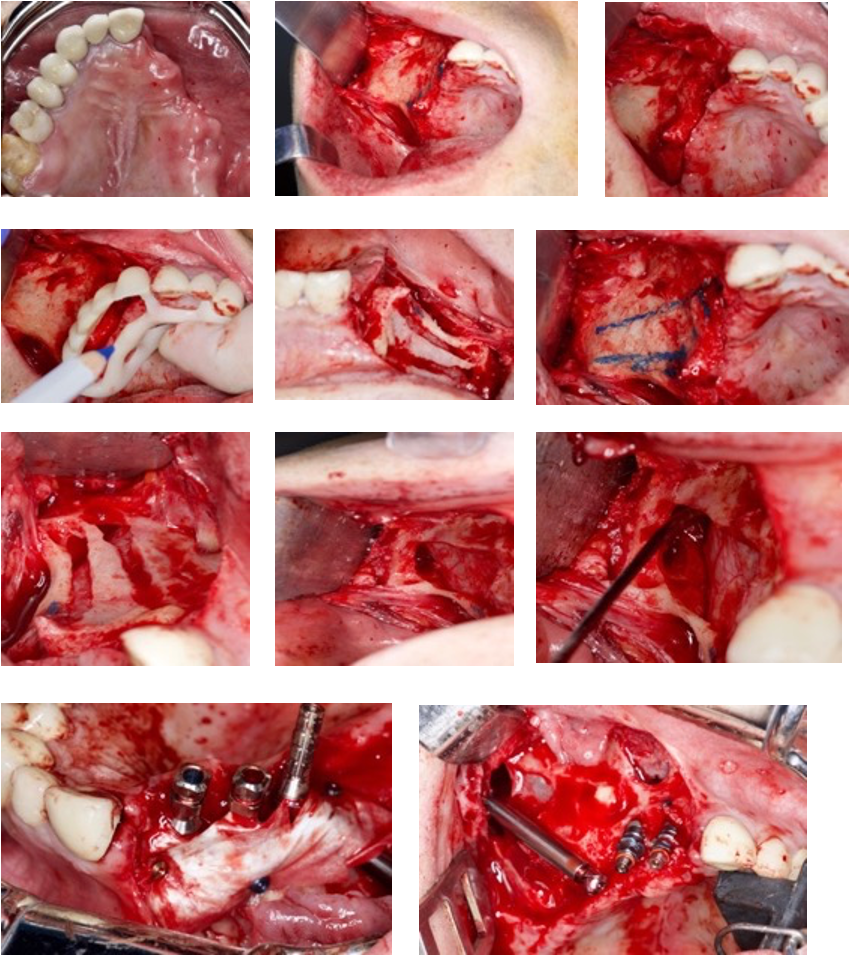
It was impossible to place the two zygomatic implants because I made a mistake when I tried to put the mesial implant with an exit towards 1.1. Therefore, there was no way to couple the implant to the manual key; the patient could not open the mouth, and it was a complication(Chrcanovic, Albrektsson and Wennerberg, 2016) for zygoma treatment.
That is why it was necessary to perform a nasal fossa elevation, place two conventional implants, and regenerate them with scraped autologous bone and 1gram Bio-Oss bone.
I covered the nostril window with a PRP(Attia et al., 2020) and the implants with a collagen membrane.
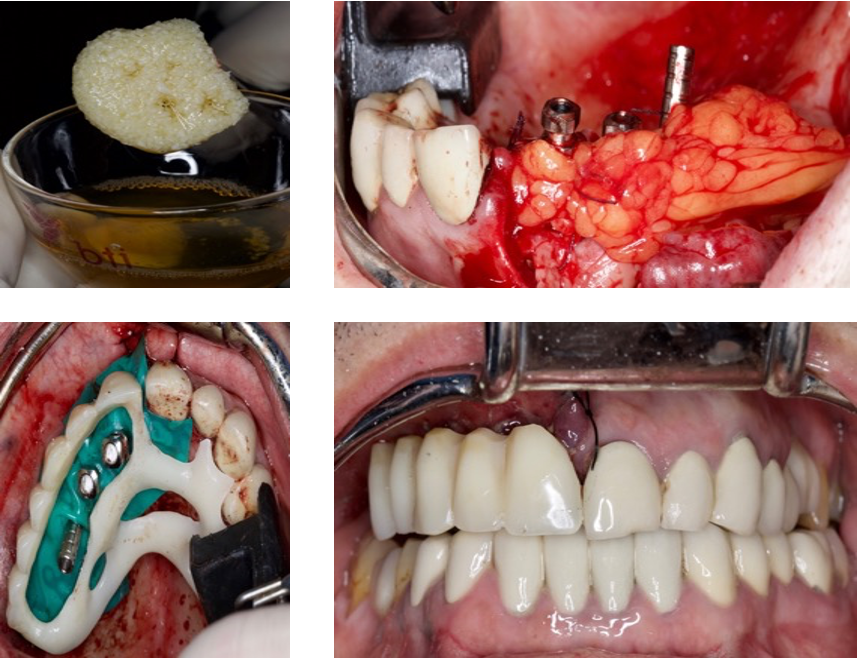
Steps to adjust temporary fixed prosthesis screwed to the implants through the provisional loading cylinders.
1. Adjust the multiunits to the torque that the manufacturer recommends. In this case, Noris medical® zygoma has 25 Ncms; for BTI® implants, it is between 15-20 Ncm for the angled ones.
2. A rubber dam protects the gum around the cylinders. Then, a white thermo-polymerizable acrylic is used, such as the Bredent® or tab 2000.
3. The prosthesis is attached to the cylinders, and we verify that none move. Then, it can be sent to the laboratory to make the final prosthesis in high-impact acrylic polish.
Suppose we have used the acrylic of high impact on the capture of the cylinders if we verify that the vertical dimension is correct, occlusion, and smile line. In that case, we can mask the prosthesis, put it in the pressure cooker, and later polish the acrylic remains.
7. Once the prosthesis is finished, it is placed on the multiunits, torqued to 15 Ncm, Teflon is placed, and it is covered with ultra-short composite.
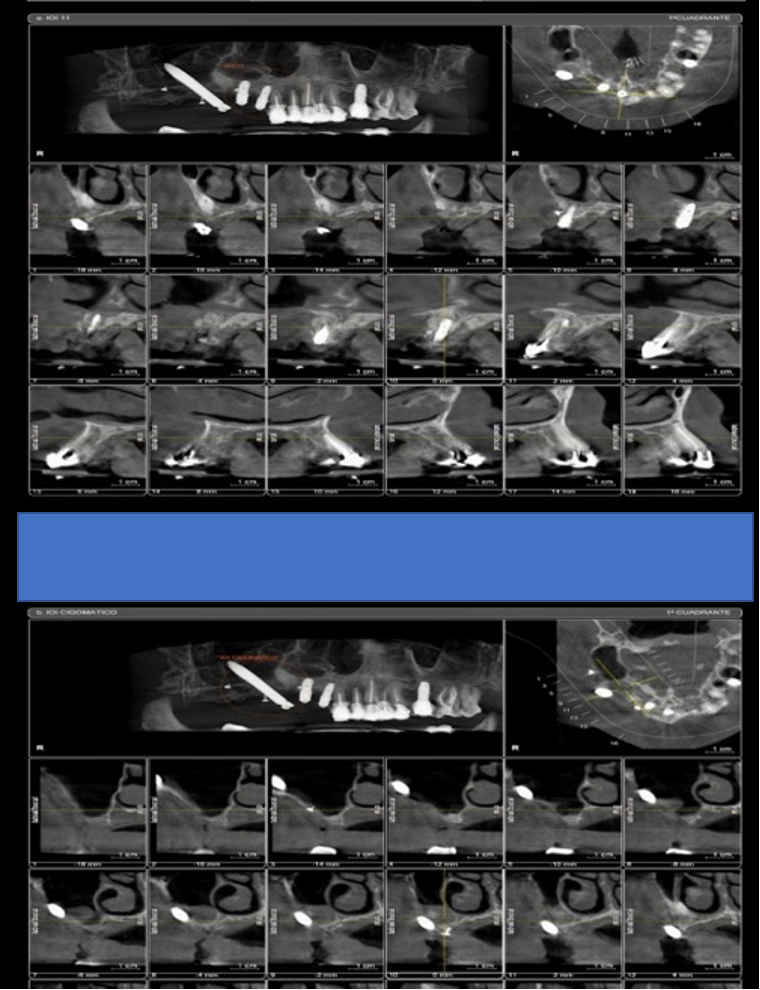
CT scan after eight months:
Periodontal re-evaluation after four months:
The aims for this treatment were completed:
A. To reduce generalized bleeding and plaque level to £25%.
B. To have a depth pocket that measures less than 5mm.
C. To eliminate pain or bad smell.
D. During these four months, the patient has not wanted to perform the endodontic treatment of pieces 2.1 and 2.2. It is warned that if it is not done, the chances of having a phlegmon with a fistula increase and that this pathology could affect implants in the future.
E. The patient has not stopped smoking or drinking; however, the teeth are stable.
In addition, the patient needs to be re-educated in oral hygiene and stop using cigarettes and drinking spiritual drinks. The patient will be scheduled in six months for periodontal maintenance if necessary.
Evolution and prognosis
In this case, the evolution and prognosis are favourable. However, when the definitive prosthesis was performed, the patient was advised to use a myorelaxant splint because it is necessary to avoid destructive occlusal forces in the implants at night.
Steps to perform fixed screw-retained definitive metal-ceramic prostheses on implants
1. The multiunits have been adjusted to the torque the manufacturer recommends; in this case, Noris medical® 25 Ncm for the zygoma and BTI® is 15-20 Ncm.
2. The impression copings are placed on the multiunits. In this case, the measurements were taken manually, not scanned. Therefore, heavy and light silicone was used to take the impression,
3. We asked for a metal test in this impression since we had the vertical dimension with the immediate temporary prosthesis, from which alginate was taken and sent as a reference.
4. Once passivity was verified, a sponge test was requested to determine if the colour and shape were adequate.
5. The next step was delivering the metal-ceramic bridge on implants and the correct use and maintenance instructions.
Photo of the metal structure after nine months post-surgery
Pictures with a definitive prosthesis

Overall
1. In this case, I learned to perform a Nasal lift with PRP plaquelet products from the patient, such as membrane or liquid PRP, to mix with the autologous and xenograft bone.
2. After nine months, the final prosthesis was made, in this case, in porcelain metal.
The patient attends a revision once every six months during the first year he wears the prosthesis and then once a year.
3. It must be maintained with perfect hygiene. In addition, it was explained that dental implants could suffer peri-implantitis and cause them to fail.
4. He was taught to use the electric toothbrush and oral irrigators.
5. The use of the shock splint at night and during the day, the anterior deprogrammer, was recommended when the patient felt clenching his teeth, but the definitive prosthesis was not ready.



