Personalized Diagnosis and Treatment in Oral Implantology
At Clínica Facialia in Silla, Valencia (Avenida Reyes Católicos, 3), we offer advanced treatments for dental implants with bone grafting, restoring chewing function and dental aesthetics in patients with severe bone atrophy. Through innovative techniques such as the Khoury technique, sinus lift, and guided bone regeneration, we achieve predictable and successful results.
Clinical Case: Complete Oral Restoration with Dental Implants and Bone Regeneration
Reason for Consultation
A 64-year-old patient, a nurse by profession, visited our clinic in Silla, Valencia, complaining of severe dental pain and mobility in teeth 3.7, 3.8, and 1.7. After a clinical and radiographic evaluation, advanced periodontal disease was detected with significant bone loss and the need for dental extractions.
Evaluation and Diagnosis
- Severe periodontal disease (Stage 3, Moderate Grade).
- Maxillary bone atrophy in quadrants 1 and 3.
- Grade 2-3 tooth mobility in several teeth.
- Presence of an impacted third molar in 4.8.
- Lack of keratinized gum in mandibular and maxillary sectors.
Treatment Plan
- Extraction of compromised teeth (3.6, 3.7, and 1.7) and elimination of periodontal pockets.
- Vertical bone regeneration surgery using the Khoury technique, utilizing the patient’s autologous bone.
- Maxillary sinus lift with a collagen membrane and the tent-pole technique with microscrews.
- Placement of dental implants after a 4-5 month bone regeneration period.
- Ramp suture technique (Tinti & Benfenati, 2002) to optimize gingival keratinization and implant aesthetics.
- Fixed prosthetic rehabilitation on implants with functional and aesthetic adjustment.
Surgical Procedure
The surgery was performed under intravenous sedation and local anaesthesia, with infiltration in the buccal area. Advanced bone regeneration techniques were used:
- Khoury Technique: Sectioning of cortical bone into two parts to create a stable three-dimensional structure.
- Sinus Lift with autograft and xenograft filling.
- Fixation with regeneration screws to consolidate the bone augmentation.
- Use of resorbable membranes to improve bone integration.
- Ramp suture technique to optimize the stability of soft tissues.
Results and Evolution
After 4 months of bone regeneration, the dental implants were successfully placed, achieving:
- Optimal bone integration and primary implant stability.
- Enhanced aesthetics with preserved gingival margins.
- Restored chewing function, avoiding removable prosthetics.
- No complications over three years of follow-up.
Benefits of Dental Implants with Bone Graft at Clínica Facialia
✅ Long-lasting and stable solution with osseointegrated implants.
Improved aesthetics and function without the need for removable prostheses.
Reduced risk of bone loss with advanced regeneration techniques.
Prevention of overly long artificial teeth, enhancing phonetics and oral hygiene.
Higher implant success rates due to the use of autologous bone.
Considerations and Risks
⚠️ Precision surgery required to avoid damage to the inferior alveolar nerve. ⚠️ Intravenous sedation with controlled risks in patients with medical histories. ⚠️ Risk of bone graft exposure, requiring specialized follow-up.
Trust the Specialists at Clínica Facialia
If you are looking for a dental implant treatment with bone grafting in Silla, Valencia, at Clínica Facialia, we have the best specialists in bone regeneration and maxillofacial surgery. We offer state-of-the-art technology and a highly trained team to ensure successful and long-term functional results.
📍 Visit us at: Avenida Reyes Católicos, 3, Silla, Valencia 📞 Contact us: Facialia.com
injerto en bloque, sutura en rampa, implantes dentales, elevacion de seno, Khoury´s technique, elevacion de seno, regeneracion osea guiada.
O.P.G before the extractions and perio-treatment:

O.P.G after two months of extractions, perio-treatment and general dentistry:

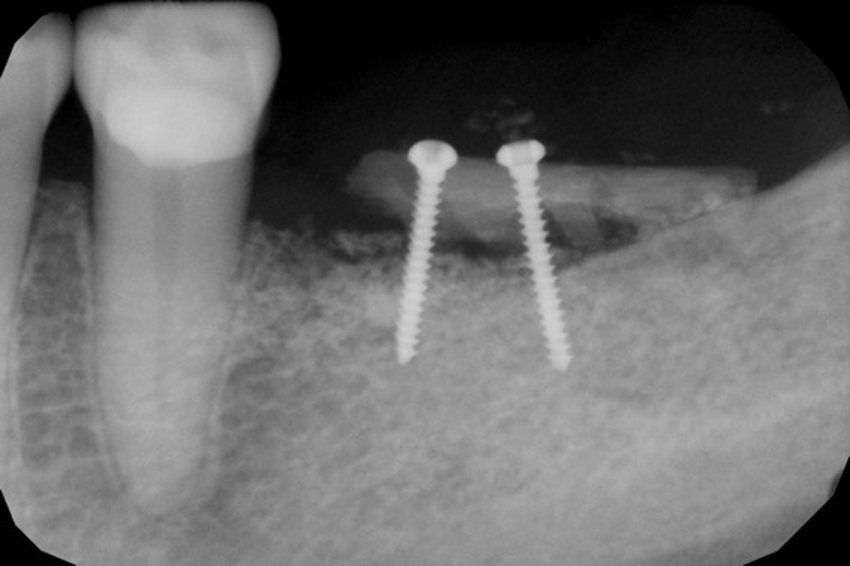
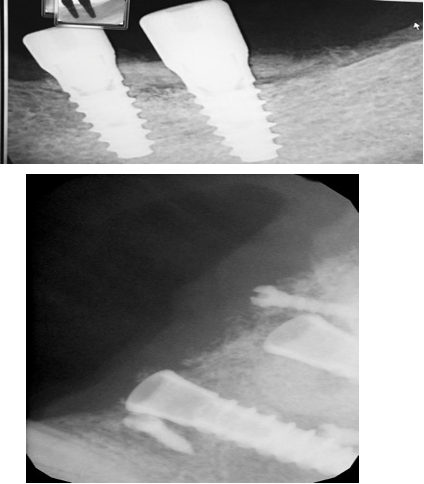
X-rays control of regeneration:
O.P.G after upper implants:

Periapical X-ray after four-month post-implants:
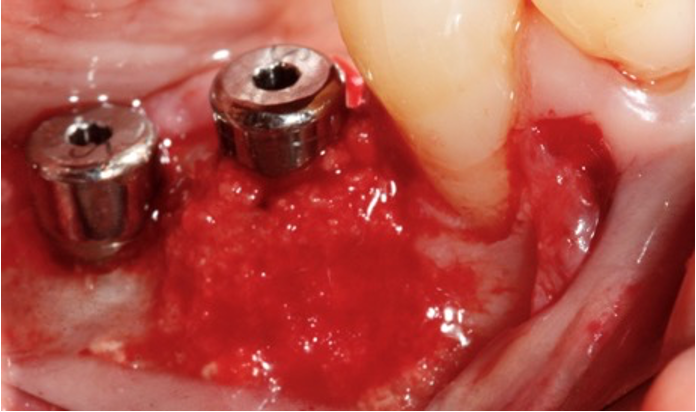
Photos after four months of bone regeneration
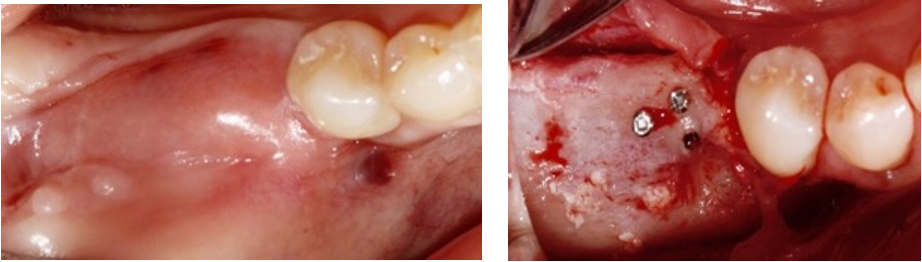
Note how the regeneration has not been entirely complete on the vestibular part. The patient does not have keratinised gum, and an apical displacement flap will have to be performed, plus a free gum graft to gain keratinised tissue or a ramp mattress suture with a connective tissue graft.
Photo with implants essential cone 0.7 from Klockner:
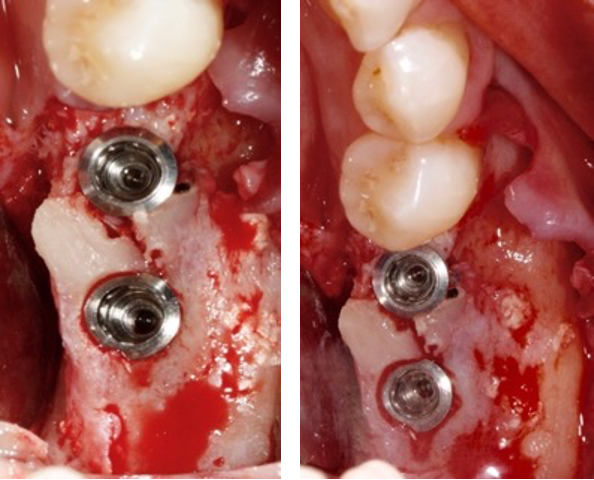
Photo of autologous bone obtained from fresh biologic drill set on the buccal side:
Ramp mattress suture:
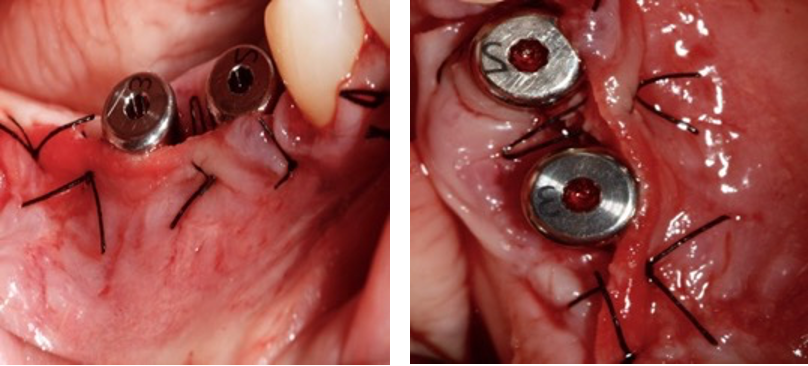
The ramp mattress suture was published by Tinti & Benfenati in 2002(Tinti, C., & Benfenati, 2002). They described the technique:
“Ramp mattress suture applies pressure and tearing forces on the flap in an apical-coronal direction at the vestibular site and opposite traction in a coronoapical order at the palatal site. The ramp mattress suture seems capable of pulling the flap in an apical-coronal direction in the vestibular area and in a coronoapical direction in the palatal site, making it possible to obtain a more coronal gingival margin.
After an adequate healing period of approximately five weeks, a vestibular scalloped gingivectomy is performed around the vestibular surface of the abutment to create either a scalloped gingival margin or interproximal papillae only in the vestibular area. Thus, forming a gingival ramp in a palate-vestibular direction to reasonably reduce the residual increased vestibular depth and optimise the aesthetic result”.
Photo of Ramp mattress suture in 1.6 and 1.7 implants after two months:

Evolution and prognosis:
The evolution and prognosis of this case have been favourable; no more teeth have been extracted in the three years I reviewed this patient.
Managing hard and soft tissues has allowed this result to be maintained over time.
Overall
In this case, it was learned to perform the tent pole technique for vertical regeneration. It was interesting to observe how sometimes the regeneration with autologous bone is not perfect, but thanks to the biological drilling, the clinical appearance of the implants could be improved. Carlo Tinti’s ramp suture helped achieve keratinised gingiva and placed it where needed. The patient attends her check-ups once a year and has not had any complications.



